Menopause is a significant biological milestone that marks the end of a woman’s reproductive years. While it is a natural process, the physical and emotional changes that accompany it can be overwhelming without proper understanding and management. The menopausal transition, also known as perimenopause, is the gradual shift leading up to menopause, characterized by fluctuating hormone levels and a variety of symptoms that can last for years. This phase affects every woman differently, with some experiencing mild discomfort while others face severe disruptions to their daily lives. By exploring what menopause and the menopausal transition entail—including symptoms, causes, diagnosis, and treatment—women can better prepare for this stage and make informed decisions about their health.
Menopause is defined as the point when a woman has not had a menstrual period for 12 consecutive months, signifying the end of her reproductive years. However, the journey to menopause—known as the menopausal transition or perimenopause—begins long before the final menstrual period. This phase typically starts in a woman’s late 40s to early 50s, though the exact timing varies based on genetics, lifestyle, and medical history. During this transition, the ovaries gradually produce less estrogen and progesterone, leading to irregular menstrual cycles and a range of symptoms such as hot flashes, mood swings, and sleep disturbances. The average age of menopause in the U.S. is 51, but some women experience it earlier (before 40) due to medical conditions, surgeries, or treatments like chemotherapy. Understanding this process is crucial because it helps women distinguish between normal changes and potential health concerns that require medical attention.
The menopausal transition is divided into three stages: perimenopause (the years leading up to menopause), menopause itself (confirmed after 12 months without a period), and postmenopause (the years following menopause). While menopause is a natural biological event, its symptoms can significantly impact quality of life, making it essential to recognize the signs early and explore effective management strategies. Women who undergo surgical menopause (due to ovary removal) experience an abrupt hormonal drop, often leading to more severe symptoms than those who transition naturally. Additionally, premature menopause (occurring before age 40) requires special medical consideration due to its association with higher risks of osteoporosis and cardiovascular disease. By educating themselves on what menopause and the menopausal transition entail, women can take proactive steps to maintain their health and well-being during this phase.
Not all women experience menopause in the same way. There are several types of menopause, each with distinct causes and implications:
Natural menopause occurs gradually as a woman ages, typically between 45 and 55 years old. It results from the ovaries slowing down their production of reproductive hormones, leading to the cessation of menstruation. This process can take several years, with perimenopause (the transitional phase) often lasting 4 to 8 years before the final menstrual period. Symptoms during this time vary widely—some women have mild discomfort, while others struggle with severe hot flashes, sleep disturbances, and emotional fluctuations. Since natural menopause is a gradual process, the body has more time to adjust to hormonal changes, which can sometimes make symptoms more manageable compared to sudden menopause caused by surgery or medical treatments.
Surgical menopause occurs when a woman undergoes removal of both ovaries (bilateral oophorectomy), leading to an immediate drop in estrogen and progesterone levels. Unlike natural menopause, which happens over years, surgical menopause triggers sudden and often more intense symptoms, including severe hot flashes, mood swings, and vaginal dryness. Women who have a hysterectomy (uterus removal) without ovary removal may not enter menopause immediately but may experience earlier menopause due to disrupted blood flow to the ovaries. Because surgical menopause accelerates bone loss and increases cardiovascular risks, hormone replacement therapy (HRT) is often recommended unless contraindicated by other health conditions.
Premature menopause (POI) occurs when a woman experiences menopause earlier than expected, typically before age 40. This condition affects about 1% of women and can result from genetic disorders (such as Turner syndrome), autoimmune diseases (like lupus or thyroid disorders), or medical treatments like chemotherapy or radiation. Women with POI may still occasionally ovulate and even conceive, but their fertility is significantly reduced. Because early menopause leads to prolonged estrogen deficiency, these women face higher risks of osteoporosis, heart disease, and cognitive decline, making early intervention with hormone therapy or other treatments crucial.
Induced menopause occurs when medical treatments—such as chemotherapy, radiation therapy, or certain medications (e.g., for endometriosis or breast cancer)—damage the ovaries and halt estrogen production. Unlike natural menopause, induced menopause can happen at any age, depending on the treatment. For example, women undergoing chemotherapy for breast cancer may experience temporary or permanent menopause, depending on their age and the drugs used. Since induced menopause can lead to abrupt and severe symptoms, doctors often recommend non-hormonal treatments (such as SSRIs for hot flashes or vaginal moisturizers for dryness) for women who cannot take estrogen due to cancer risks.
Understanding these types of menopause helps women and healthcare providers tailor treatment plans based on individual needs, whether managing natural hormonal decline or addressing sudden menopause due to medical interventions.
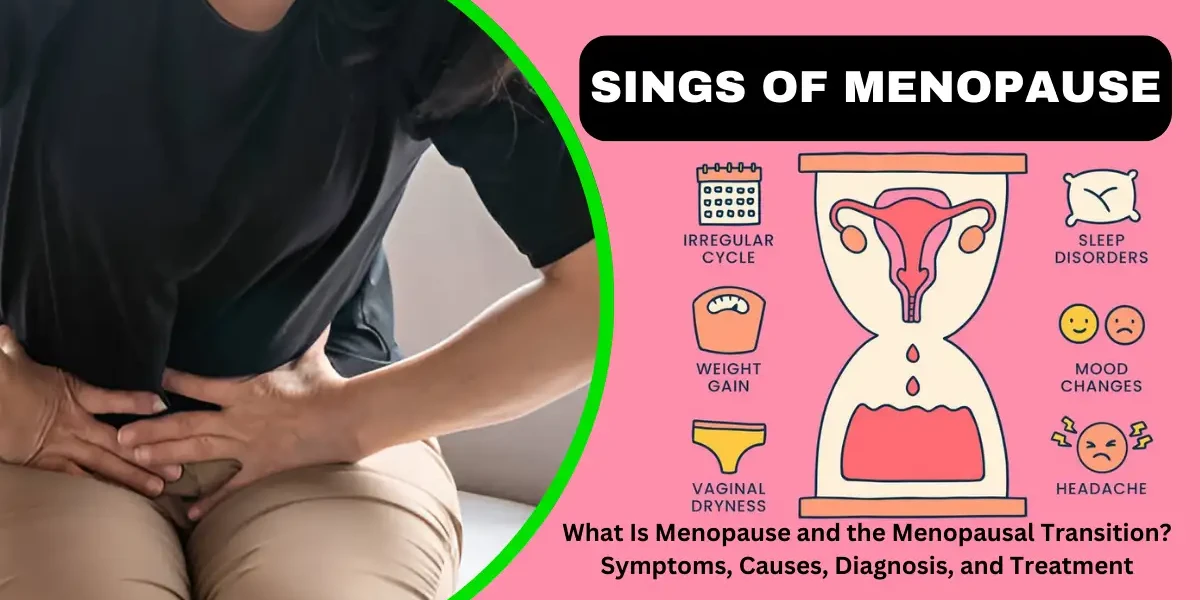
Menopause and perimenopause are natural biological processes that mark the end of a woman’s reproductive years. Perimenopause refers to the transitional phase leading up to menopause, during which the body undergoes hormonal fluctuations, primarily a decline in estrogen and progesterone. A formal menopause diagnosis is confirmed once a woman has not had a menstrual cycle for 12 straight months. Both stages are associated with a wide range of signs and symptoms, which can vary in severity and duration from woman to woman. Understanding these symptoms is crucial for managing them effectively and maintaining quality of life during this transition.
1. Irregular Menstrual Cycles
One of the earliest and most noticeable signs of perimenopause is a change in menstrual patterns. Periods may become irregular—shorter, longer, heavier, or lighter—before eventually stopping altogether. Some women experience skipped cycles, while others may have frequent bleeding. These irregularities occur due to fluctuating hormone levels, particularly estrogen and progesterone, which regulate the menstrual cycle.
2. Hot Flashes and Night Sweats
Hot flashes are among the most common and bothersome symptoms, affecting about 75% of women during perimenopause and menopause. A hot flash is a sudden sensation of intense heat, often accompanied by sweating, flushing (redness of the face and neck), and a rapid heartbeat. These episodes can last from a few seconds to several minutes and may occur multiple times a day. Night sweats are hot flashes that happen during sleep, often leading to disrupted sleep and fatigue. The exact cause of hot flashes is not fully understood, but they are believed to be related to changes in the hypothalamus (the body’s temperature regulator) due to declining estrogen levels.
3. Sleep Disturbances
Many women report difficulty sleeping during perimenopause and menopause. This can be due to night sweats, hormonal fluctuations, or increased anxiety. Insomnia, frequent waking, and trouble falling asleep are common complaints. Poor sleep quality can contribute to daytime fatigue, irritability, and difficulty concentrating.
4. Mood Changes and Emotional Symptoms
Hormonal shifts can significantly impact mood, leading to irritability, anxiety, depression, and mood swings. Estrogen plays a role in regulating serotonin and dopamine, neurotransmitters that influence mood. As estrogen levels drop, some women experience heightened emotional sensitivity, feelings of sadness, or even clinical depression. Stress and life changes during midlife (such as aging parents or career pressures) can exacerbate these symptoms.
5. Vaginal Dryness and Atrophy
Declining estrogen levels cause changes in vaginal tissue, leading to vaginal dryness, itching, and discomfort. The vaginal walls may become thinner and less elastic (a condition called vaginal atrophy), making sexual intercourse painful (dyspareunia). Some women also experience an increased risk of urinary tract infections (UTIs) due to changes in the urinary tract lining.
6. Decreased Libido (Sexual Desire)
Many women notice a decline in sexual desire during perimenopause and menopause. This can be due to hormonal changes, vaginal dryness, fatigue, or emotional factors such as stress or body image concerns. Testosterone, which contributes to libido, also decreases with age, further affecting sexual interest.
7. Weight Gain and Metabolic Changes
Hormonal shifts can slow metabolism, leading to weight gain, particularly around the abdomen. Muscle mass may decrease while fat storage increases, making it harder to maintain previous weight levels. Insulin resistance can also develop, increasing the risk of type 2 diabetes.
8. Thinning Hair and Dry Skin
Estrogen helps maintain collagen and skin elasticity. As levels drop, women may notice dry skin, thinning hair, and brittle nails. Some experience hair loss or increased facial hair due to a relative increase in androgens (male hormones) like testosterone.
9. Memory Problems and Difficulty Concentrating ("Brain Fog")
Many women report forgetfulness, difficulty focusing, and mental fog during perimenopause and menopause. Estrogen supports brain function, and its decline may affect memory and cognitive performance. Sleep disturbances and stress can also contribute to these symptoms.
10. Joint and Muscle Pain
Some women experience increased joint stiffness, aches, and muscle pain during menopause. Estrogen has anti-inflammatory properties, and its reduction may contribute to conditions like osteoarthritis.
11. Headaches and Migraines
Women with a history of hormonal migraines may notice changes in headache patterns during perimenopause. Fluctuating estrogen levels can trigger more frequent or severe migraines.
12. Heart Palpitations
Some women report episodes of rapid or irregular heartbeat during menopause. While usually harmless, these palpitations can be alarming and are often linked to hormonal changes affecting the autonomic nervous system.
13. Changes in Urinary Function
Weakened pelvic floor muscles and thinning urethral tissues can lead to urinary incontinence (leakage when coughing, sneezing, or exercising) or increased urinary frequency.
14. Bone Density Loss (Osteoporosis Risk)
Estrogen helps protect bone density. After menopause, bone loss accelerates, increasing the risk of osteoporosis and fractures. Regular weight-bearing exercise and calcium/vitamin D intake are essential for prevention.
The most common cause of menopause is the natural aging process of the ovaries. Women are born with a finite number of eggs (approximately 1-2 million at birth), which gradually deplete over time through ovulation and follicular atresia (natural degeneration). As a woman approaches her late 30s and 40s, the ovaries produce less estrogen and progesterone, the hormones responsible for regulating menstruation and ovulation. This decline leads to irregular menstrual cycles before they eventually stop altogether. The perimenopausal transition—the years leading up to menopause—is characterized by fluctuating hormone levels, which contribute to symptoms like hot flashes, night sweats, and mood changes.
Unlike natural menopause, which occurs gradually, surgical menopause happens immediately when both ovaries are removed. Since the ovaries are the primary source of estrogen and progesterone, their removal causes an abrupt hormonal drop, leading to severe and sudden menopausal symptoms. Women who undergo this procedure before natural menopause often experience more intense symptoms, including severe hot flashes, vaginal dryness, and an increased risk of osteoporosis and cardiovascular disease due to the loss of estrogen's protective effects. A hysterectomy (removal of the uterus) without oophorectomy does not cause menopause, as the ovaries continue producing hormones, but it does stop menstruation.
Cancer treatments such as chemotherapy and pelvic radiation can damage ovarian follicles, leading to premature menopause. The likelihood depends on the type and dosage of chemotherapy drugs, as well as the woman's age at the time of treatment. Alkylating agents, commonly used in breast cancer and lymphoma treatments, are particularly toxic to the ovaries. Radiation therapy targeting the pelvic area (for cervical, uterine, or rectal cancers) can also destroy ovarian tissue. Some women may experience temporary ovarian suppression, with periods returning after treatment, while others face permanent menopause. Fertility preservation options, such as egg freezing or ovarian suppression medications, may be considered before undergoing such treatments.
Premature ovarian insufficiency (POI), also known as premature menopause, occurs when the ovaries stop functioning before age 40. This condition affects about 1% of women and can result from genetic disorders like Turner syndrome (a chromosomal abnormality where one X chromosome is missing or incomplete) or Fragile X premutation (a genetic mutation affecting ovarian reserve). Autoimmune diseases, such as thyroiditis or lupus, may also cause the immune system to attack ovarian tissue. In some cases, POI is idiopathic, meaning no clear cause is identified. Women with POI often require hormone replacement therapy (HRT) to mitigate symptoms and reduce long-term health risks like osteoporosis and heart disease.
Certain lifestyle choices and environmental exposures can influence the timing of menopause:
Smoking: Chemicals in cigarettes, such as nicotine and polycyclic aromatic hydrocarbons, are toxic to ovarian follicles. Studies show that smokers reach menopause 1-2 years earlier than non-smokers.
Body Weight: Adipose (fat) tissue produces small amounts of estrogen. Women with very low body fat (e.g., athletes or those with eating disorders) may experience earlier menopause due to lower estrogen levels, while obese women may have a slightly delayed menopause.
Alcohol Consumption: Moderate alcohol intake has been linked to a later onset of menopause, possibly due to its effect on estrogen metabolism. However, excessive drinking can have adverse health effects.
Environmental Toxins: Exposure to endocrine-disrupting chemicals (e.g., phthalates in plastics, pesticides, and industrial pollutants) may accelerate ovarian aging.
Number of Pregnancies: Women who have never been pregnant may experience menopause later, possibly due to more remaining ovarian follicles.
Age at Menarche: Early menstruation (before age 11) has been associated with later menopause, while late menarche may slightly increase the risk of early menopause.
Chronic Illnesses: Conditions like diabetes, epilepsy, and autoimmune disorders (e.g., rheumatoid arthritis) are linked to earlier menopause, possibly due to systemic inflammation or hormonal disruptions.
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It occurs in three main stages: perimenopause, menopause, and postmenopause. Each stage has distinct hormonal changes, symptoms, and health implications.
1. Perimenopause (The Transition Phase)
Perimenopause, often called the menopausal transition, typically begins in a woman’s 40s but can start earlier for some. During this phase, the ovaries gradually produce less estrogen, leading to irregular menstrual cycles. Females might encounter signs like sudden warmth, nocturnal perspiration, emotional fluctuations, disrupted sleep, and vaginal moisture loss. Reproductive capability diminishes, though conception remains feasible until menopause is officially reached. This stage can last anywhere from a few months to over a decade, with symptoms varying in intensity.
2. Menopause (The Cessation of Periods)
Menopause is officially diagnosed when a woman has gone 12 consecutive months without a menstrual period, marking the end of ovulation and fertility. The average age for menopause is 51, but it can occur earlier due to genetics, surgery (such as a hysterectomy), or medical treatments like chemotherapy. Estrogen and progesterone levels drop significantly, which can lead to more pronounced symptoms, including increased hot flashes, bone density loss (raising osteoporosis risk), weight gain, and changes in cholesterol levels. Some women also experience cognitive changes, such as memory lapses or difficulty concentrating.
3. Postmenopause (The Years After Menopause)
Postmenopause refers to the years following menopause, during which menopausal symptoms may lessen but long-term health effects become more significant. Due to low estrogen levels, women face higher risks of osteoporosis, heart disease, and urinary incontinence. Maintaining a healthy lifestyle—through a balanced diet, regular exercise, calcium and vitamin D supplementation, and routine health screenings—is crucial during this stage. Hormone replacement therapy (HRT) or other treatments may be recommended to manage persistent symptoms and reduce health risks.
While often used interchangeably, these terms describe distinct phases with important differences:
| Characteristic | Perimenopause | Menopause |
|---|---|---|
| Timing | 4-10 years before final period | Starts after 12 period-free months |
| Hormone Status | Erratic highs and lows | Consistently low |
| Fertility | Possible but declining | Zero |
| Symptom Intensity | Often worst in late perimenopause | May improve after 2-3 years |
| Medical Focus | Symptom management | Long-term health protection |
Real-world example:
A 47-year-old with irregular periods and hot flashes is in perimenopause. Her 54-year-old sister who hasn’t bled in 18 months is postmenopausal—even if she still has occasional flashes.
Why the distinction matters:
Treatment approaches differ (e.g., birth control may help in perimenopause but not postmenopause)
Health risks change (bone loss accelerates after menopause)
Psychological impact varies (the transition phase often feels most disruptive)
Diagnosing menopause typically involves evaluating a woman’s symptoms, medical history, and sometimes laboratory tests. Since menopause is a natural biological process, doctors often rely on clinical signs rather than extensive testing. However, in some cases, diagnostic tests may be necessary, especially if menopause occurs earlier than expected or if symptoms are unclear.
1. Assessment of Symptoms
The most common indicator of menopause is the presence of characteristic symptoms, such as irregular periods, hot flashes, night sweats, vaginal dryness, mood swings, and sleep disturbances. A healthcare provider will review these symptoms along with the patient’s menstrual history. If a woman over the age of 45 experiences these signs along with irregular cycles, it is often sufficient to confirm perimenopause or menopause without further testing.
2. Medical and Menstrual History
A detailed medical and menstrual history helps determine whether a woman is transitioning into menopause. The doctor may ask about the frequency and duration of menstrual cycles, changes in bleeding patterns, and any related health conditions. Family history of early menopause or surgical interventions (such as hysterectomy or ovary removal) can also influence the diagnosis.
3. Hormone Level Testing
In some cases, blood tests may be conducted to measure hormone levels, particularly follicle-stimulating hormone (FSH) and estrogen (estradiol). FSH levels tend to rise as ovarian function declines, while estradiol levels drop. However, hormone levels can fluctuate during perimenopause, so a single test may not be conclusive. Testing is more useful for women under 45 with suspected premature menopause or those who have had a hysterectomy but retained their ovaries.
4. Ruling Out Other Conditions
Since symptoms like irregular periods and fatigue can be caused by other conditions (e.g., thyroid disorders, polycystic ovary syndrome, or hormonal imbalances), doctors may perform additional tests to exclude these possibilities. Thyroid function tests, prolactin levels, and pelvic ultrasounds may be used if symptoms are atypical.
5. Confirming Menopause in Special Cases
For women who have undergone surgical menopause (removal of ovaries) or chemotherapy-induced menopause, the diagnosis is straightforward due to the sudden drop in hormone production. In such cases, symptoms usually appear abruptly, and hormone testing may not be necessary.
Menopause is a natural biological transition that marks the end of a woman’s reproductive years, typically occurring between ages 45 and 55. As ovarian function declines, estrogen and progesterone levels drop, leading to a variety of symptoms such as hot flashes, night sweats, vaginal dryness, mood changes, sleep disturbances, and an increased risk of osteoporosis. Managing these symptoms effectively requires a personalized approach, incorporating hormone therapy, non-hormonal medications, lifestyle changes, and alternative treatments. This guide provides an in-depth exploration of the available treatment options to help women make informed decisions about their health during menopause.
Types of Hormone Therapy
Hormone therapy (HT) remains the gold standard for treating moderate to severe menopausal symptoms, particularly hot flashes, night sweats, and vaginal atrophy. There are two main types of HT:
Estrogen-Only Therapy (ET): Recommended for women who have had a hysterectomy (surgical removal of the uterus). Estrogen can be administered orally, through transdermal patches, gels, or sprays.
Combined Estrogen-Progestin Therapy (EPT): Necessary for women who still have a uterus because estrogen alone can increase the risk of endometrial cancer. Progestin (synthetic progesterone) or micronized progesterone (a bioidentical form) is added to protect the uterine lining.
Benefits of Hormone Therapy
HT is highly effective in alleviating vasomotor symptoms (hot flashes and night sweats), reducing their frequency and severity by up to 90%. It also helps restore vaginal moisture and elasticity, decreasing discomfort during intercourse. Additionally, HT plays a crucial role in preventing bone loss and reducing fracture risk in postmenopausal women. Some studies suggest that early initiation of HT (within 10 years of menopause) may also have cardiovascular benefits, though this remains a debated topic.
Risks and Considerations
While HT is beneficial, it is not without risks. Long-term use of combined estrogen-progestin therapy has been associated with a slightly increased risk of breast cancer, blood clots, and stroke. Oral estrogen carries a higher risk of venous thromboembolism compared to transdermal forms. Women with a history of breast cancer, cardiovascular disease, or blood clots are generally advised against systemic HT. The decision to use HT should be based on individual risk factors, symptom severity, and patient preferences, with regular follow-ups to reassess its necessity.
For women who cannot or prefer not to use hormone therapy, several non-hormonal medications can help manage menopausal symptoms.
A. SSRIs and SNRIs for Hot Flashes and Mood Disorders
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), commonly used as antidepressants, have been found effective in reducing hot flashes. Paroxetine (Brisdelle) is the only FDA-approved SSRI specifically for menopausal hot flashes. Venlafaxine (Effexor) and escitalopram (Lexapro) are also frequently prescribed off-label. These medications can improve mood swings, anxiety, and irritability while reducing the frequency of vasomotor symptoms.
B. Gabapentin and Pregabalin for Night Sweats and Sleep Disturbances
Originally developed for nerve pain and seizures, gabapentin (Neurontin) and pregabalin (Lyrica) have shown efficacy in reducing night sweats and improving sleep quality. These drugs work by modulating nerve activity, which may help regulate body temperature fluctuations. They are particularly useful for women who cannot take hormones or SSRIs.
C. Ospemifene for Vaginal Dryness
Ospemifene (Osphena) is a selective estrogen receptor modulator (SERM) that mimics estrogen’s effects on vaginal tissue without stimulating the uterus or breasts. It is an excellent option for women experiencing painful intercourse due to vaginal atrophy but who cannot use traditional estrogen therapy.
Many women experience vaginal dryness, itching, and discomfort during menopause due to decreased estrogen levels. Systemic hormone therapy may not be necessary if symptoms are limited to the vaginal area. Local estrogen therapy provides relief with minimal systemic absorption, making it a safer long-term option. Available forms include:
Vaginal creams (Estrace, Premarin)
Vaginal tablets (Vagifem)
Estrogen rings (Estring)
These treatments restore vaginal moisture and elasticity, reducing pain during intercourse and urinary discomfort.
Some women prefer natural or non-pharmaceutical approaches to manage menopause symptoms. While evidence varies, the following options may provide relief for some individuals:
A. Phytoestrogens (Soy, Flaxseed, Red Clover): Phytoestrogens are plant-derived compounds that mimic weak estrogen effects in the body. Soy isoflavones and flaxseed lignans are commonly used to alleviate mild hot flashes. However, research results are mixed, and their effectiveness may depend on individual metabolism.
B. Black Cohosh: Black cohosh, an herbal supplement, is widely used in Europe for menopause symptoms. Some studies suggest it may reduce hot flashes, while others show no significant benefit. Its exact mechanism remains unclear, and long-term safety data are limited.
C. Bioidentical Hormones: Bioidentical hormones are chemically identical to those produced by the human body and are often marketed as a "natural" alternative to traditional HT. However, compounded bioidentical hormones (custom-mixed by pharmacies) are not FDA-regulated, raising concerns about consistency and safety. FDA-approved bioidentical options, such as estradiol patches and micronized progesterone, are considered safer choices.
Menopause accelerates bone loss, increasing the risk of osteoporosis and fractures. Preventive and therapeutic strategies include:
A. Bisphosphonates (Alendronate, Risedronate, Zoledronic Acid): These drugs slow bone breakdown and are first-line treatments for osteoporosis. They can be taken orally (weekly or monthly) or intravenously (yearly).
B. Denosumab (Prolia): A monoclonal antibody given as a twice-yearly injection, denosumab inhibits bone resorption and is highly effective in preventing fractures.
C. Calcium and Vitamin D Supplementation: Adequate calcium (1200 mg/day) and vitamin D (800–1000 IU/day) intake is essential for maintaining bone density. Women with limited sun exposure or dietary deficiencies may require higher doses.
In addition to medical treatments, lifestyle changes can significantly improve menopause symptoms:
A. Regular Exercise: Weight-bearing exercises (walking, strength training) help maintain bone density, while yoga and Pilates improve flexibility and reduce stress.
B. Balanced Diet: A diet rich in calcium, vitamin D, omega-3 fatty acids, and phytoestrogens supports overall health. Reducing caffeine, alcohol, and spicy foods may help minimize hot flashes.
C. Stress Reduction Techniques: Mindfulness meditation, deep breathing exercises, and cognitive behavioral therapy (CBT) can alleviate mood swings and sleep disturbances.
Menopause is a normal physiological transition signaling the conclusion of a woman's fertility, usually happening between 45 and 55 years of age. This transition is characterized by a decline in estrogen and progesterone production, leading to various physical and psychological symptoms. While hormone replacement therapy (HRT) and lifestyle modifications are common management strategies, exercise stands out as one of the most effective non-pharmacological interventions. This article explores the profound impact of exercise on menopausal symptoms, bone health, cardiovascular function, mental well-being, and overall quality of life.
One of the most noticeable effects of menopause is weight gain, particularly around the abdomen. This shift is partly due to hormonal changes that slow metabolism and redistribute fat storage. Additionally, aging naturally reduces muscle mass, further decreasing calorie expenditure.
How Exercise Helps:
Aerobic Exercise: Activities like brisk walking, jogging, cycling, and swimming increase calorie burn, helping to prevent weight gain. Studies show that 30-60 minutes of moderate-intensity cardio most days of the week can counteract menopausal weight gain.
Strength Training: Resistance exercises (weight lifting, resistance bands, bodyweight exercises) preserve lean muscle mass, which is crucial for maintaining metabolic rate. Muscle tissue burns more calories at rest than fat, making strength training essential for long-term weight control.
High-Intensity Interval Training (HIIT): Short bursts of intense exercise followed by recovery periods have been shown to effectively reduce abdominal fat and improve insulin sensitivity, which can decline during menopause.
Estrogen plays a vital role in maintaining bone density. As levels drop during menopause, bone resorption outpaces formation, increasing the risk of osteoporosis and fractures.
How Exercise Helps:
Weight-Bearing Exercises: Walking, dancing, hiking, and stair climbing stimulate bone remodeling, enhancing density in the hips and spine.
Resistance Training: Lifting weights or using resistance machines applies stress to bones, promoting mineralization and strength. Research indicates that women who engage in regular strength training maintain higher bone density post-menopause.
Balance and Flexibility Work: Yoga and tai chi improve posture and coordination, reducing fall risk—a critical factor in preventing fractures in osteoporotic individuals.
Before menopause, estrogen provides some protection against heart disease by maintaining healthy cholesterol levels and blood vessel flexibility. Post-menopause, women’s cardiovascular risk rises to match that of men.
How Exercise Helps:
Aerobic Exercise: Lowers LDL (“bad”) cholesterol, raises HDL (“good”) cholesterol, and improves blood pressure.
Endothelial Function: Physical activity enhances blood vessel dilation, improving circulation and reducing hypertension risk.
Reduced Inflammation: Regular exercise decreases systemic inflammation, a key contributor to atherosclerosis.
Menopause can bring mood swings, irritability, anxiety, and even depression due to hormonal shifts and life stressors.
How Exercise Helps:
Endorphin Release: Physical activity triggers the release of endorphins, natural mood lifters that combat stress and depression.
Stress Reduction: Yoga and mindfulness-based exercises lower cortisol levels, promoting relaxation.
Improved Sleep: Many menopausal women struggle with insomnia. Regular exercise regulates circadian rhythms and reduces nighttime hot flashes, leading to deeper, more restorative sleep.
Though the exact mechanism isn’t fully understood, studies suggest that active women experience fewer and less severe hot flashes. Exercise improves thermoregulation by enhancing the body’s ability to dissipate heat.
Aerobic Exercise: 150 minutes per week of moderate activity (e.g., brisk walking) or 75 minutes of vigorous activity (e.g., running).
Strength Training: 2-3 sessions per week, targeting major muscle groups.
Flexibility & Balance: Daily stretching or yoga to maintain mobility.
Exercise is a powerful tool for navigating the menopausal transition. It mitigates weight gain, strengthens bones, protects the heart, uplifts mood, and improves sleep. By adopting a consistent, varied exercise regimen, women can enhance their quality of life during and beyond menopause. Always consult a healthcare provider before starting a new fitness program, especially if pre-existing conditions are present.
Menopause, the natural cessation of menstruation, marks the end of a woman's reproductive years. While it is a normal biological process, it can lead to several physical and psychological complications due to hormonal changes, primarily the decline in estrogen and progesterone levels. These complications can significantly impact a woman's quality of life and long-term health.
1. Cardiovascular Disease
The decline in estrogen levels during menopause increases the risk of cardiovascular diseases, including hypertension, atherosclerosis, and heart disease. Estrogen helps maintain healthy blood vessels by promoting flexibility and regulating cholesterol levels. After menopause, women experience unfavorable changes in lipid profiles, such as increased LDL ("bad" cholesterol) and decreased HDL ("good" cholesterol), leading to a higher risk of heart attacks and strokes. Additionally, blood pressure tends to rise, further contributing to cardiovascular risks. Regular exercise, a heart-healthy diet, and medical monitoring are essential to mitigate these risks.
2. Osteoporosis and Bone Fractures
Estrogen plays a crucial role in maintaining bone density by inhibiting bone resorption. Postmenopausal women experience accelerated bone loss, increasing the risk of osteoporosis and fractures, particularly in the hips, spine, and wrists. Studies show that women can lose up to 20% of their bone density in the first five to seven years after menopause. To prevent severe bone deterioration, doctors often recommend calcium and vitamin D supplements, weight-bearing exercises, and, in some cases, hormone replacement therapy (HRT) or other bone-strengthening medications.
3. Weight Gain and Metabolic Changes
Many women notice weight gain, particularly around the abdomen, during menopause due to hormonal fluctuations, aging, and decreased muscle mass. This shift in fat distribution is linked to a higher risk of insulin resistance, metabolic syndrome, and type 2 diabetes. Slower metabolism and lifestyle factors further contribute to these changes. Managing weight through a balanced diet, regular physical activity, and strength training can help reduce these risks.
4. Genitourinary Syndrome of Menopause (GSM)
GSM encompasses various urogenital symptoms caused by decreased estrogen, including vaginal dryness, itching, painful intercourse (dyspareunia), and recurrent urinary tract infections (UTIs). The thinning of vaginal tissues (vaginal atrophy) and reduced lubrication can lead to discomfort and sexual dysfunction. Additionally, weakened pelvic muscles may contribute to urinary incontinence. Treatments include vaginal moisturizers, lubricants, low-dose vaginal estrogen therapy, and pelvic floor exercises.
5. Mood Disorders and Cognitive Changes
Hormonal fluctuations during menopause can trigger mood swings, anxiety, depression, and irritability. Sleep disturbances due to night sweats and insomnia further exacerbate emotional instability. Some women also report memory lapses, difficulty concentrating, and a higher risk of cognitive decline later in life. While the exact link between menopause and cognitive changes is still being studied, maintaining mental health through therapy, stress management, and, if necessary, antidepressants or HRT can be beneficial.
6. Increased Risk of Certain Cancers
Postmenopausal women face a higher risk of breast and ovarian cancers, partly due to prolonged exposure to estrogen (especially in cases of late menopause or hormone therapy use). Additionally, obesity after menopause increases the likelihood of endometrial cancer. Regular screenings, such as mammograms and pelvic exams, along with a healthy lifestyle, are crucial for early detection and prevention.
Menopause represents not just an ending of reproductive capacity, but the beginning of a new life phase filled with both challenges and opportunities. The menopausal transition affects every woman differently, but armed with comprehensive knowledge about symptoms, treatment options, and long-term health considerations, women can navigate this change with confidence rather than apprehension.
The most successful approaches combine:
Medical interventions when appropriate
Lifestyle modifications tailored to individual needs
Psychological support to address emotional changes
Preventive healthcare to protect future wellbeing
Perhaps most importantly, the cultural narrative around menopause is shifting. No longer viewed as a deficiency or disorder, modern medicine now recognizes menopause as a natural biological process that, when properly managed, need not limit a woman's quality of life or aspirations. With the right strategies, many women find postmenopausal years to be among their most productive and fulfilling.
Future directions in menopause care include:
Personalized hormone therapy approaches
Advanced non-hormonal treatments
Better integration of mental health support
Increased focus on sexual health preservation
By staying informed and proactive, women can transform the menopausal transition from a time of uncertainty to one of empowerment and renewed vitality. The key lies in recognizing that while menopause is inevitable, suffering through it is not - excellent care and support can make all the difference.
The 5 pillars of menopause (key areas to focus on for managing symptoms) are:
Nutrition (balanced diet rich in phytoestrogens, calcium, and vitamins)
Exercise (strength training, cardio, and flexibility exercises)
Sleep (prioritizing quality sleep to manage fatigue and mood swings)
Stress Management (mindfulness, yoga, meditation)
Hormonal & Medical Support (HRT, supplements, or alternative therapies)
The 5 stages of menopause are:
Premenopause – Regular menstrual cycles, no symptoms.
Perimenopause (early & late) – Hormonal fluctuations, irregular periods, and symptoms like hot flashes.
Menopause – Defined as 12 months without a period.
Postmenopause (early & late) – Symptoms may continue but often decrease over time.
Late Postmenopause – Long-term health considerations (bone density, heart health).
3. What is the difference between perimenopause and menopause transition?
Perimenopause is the entire phase leading up to menopause, marked by hormonal changes and symptoms (can last 4-10 years).
Menopause transition is a subset of perimenopause, specifically the later stage when periods become very irregular and symptoms intensify.
The average age for menopause is 51, but it can occur between 45-55. Early menopause (before 40) is called premature menopause.
The main problem is hormonal imbalance (declining estrogen and progesterone), leading to symptoms like hot flashes, mood swings, sleep disturbances, and long-term risks (osteoporosis, heart disease).
The most common and prominent symptom is hot flashes (sudden heat, sweating, and flushing).
Long-term risks include:
Osteoporosis (bone loss due to low estrogen)
Cardiovascular disease (increased risk of heart issues)
Weight gain & metabolic changes
Mood disorders (anxiety, depression)
Vaginal atrophy & urinary issues
Some effective natural remedies include:
Black cohosh (for hot flashes)
Flaxseeds & soy (phytoestrogens)
Magnesium & vitamin D (bone health)
Yoga & meditation (stress relief)
Evening primrose oil (mood & skin health)
The best fruits for menopause are:
Soy-based foods (edamame, tofu) – contain phytoestrogens
Berries (blueberries, strawberries) – antioxidants
Flaxseeds (lignans for hormone balance)
Avocados (healthy fats for hormone production)
Citrus fruits (vitamin C for collagen & skin health)
The strongest natural estrogen-like compounds are:
Genistein & Daidzein (found in soy and red clover)
Lignans (flaxseeds, sesame seeds)
Resveratrol (red grapes, berries)
Best menopause-friendly drinks:
Soy milk (phytoestrogens)
Green tea (antioxidants, may help hot flashes)
Water with lemon (hydration & digestion)
Maca root latte (hormone-balancing adaptogen)
Chamomile tea (calming, aids sleep)