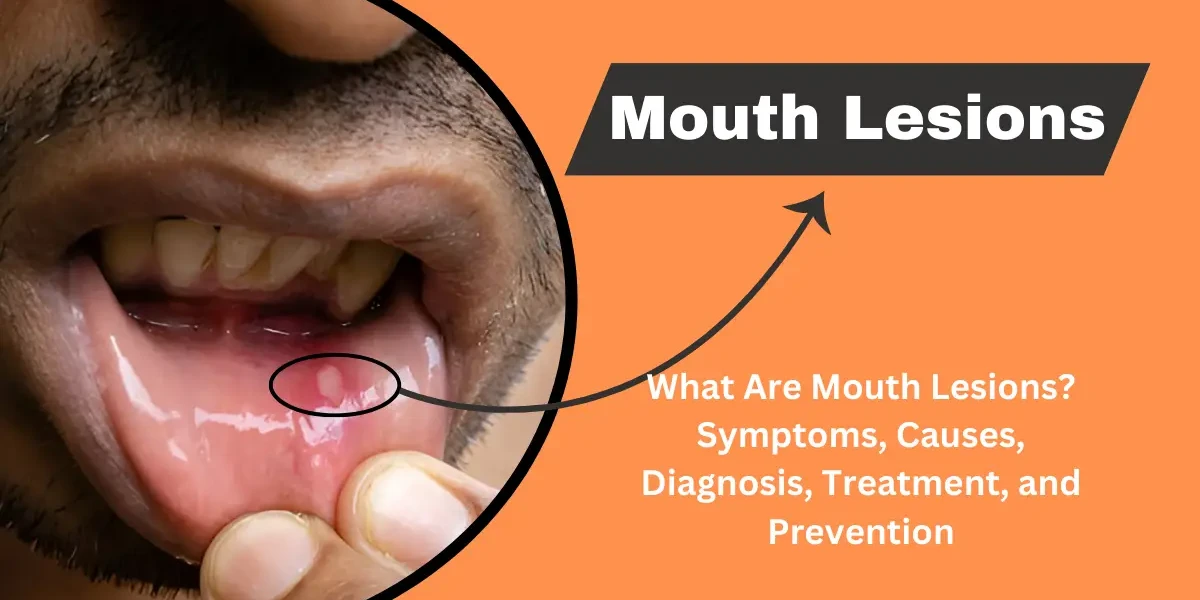
Mouth lesions are abnormal growths, ulcers, or discolorations that appear on the soft tissues of the mouth, including the lips, gums, tongue, cheeks, and palate. They can range from harmless canker sores to more serious conditions like oral cancer. Understanding the types of mouth lesions, their symptoms and signs, causes and risk factors, and available treatment and prevention methods is essential for maintaining good oral health.
Mouth lesions are abnormal growths, sores, or ulcers that develop in the oral cavity, including the lips, tongue, gums, inner cheeks, and palate. These lesions can vary in size, color, and texture, and may cause pain, discomfort, or difficulty in eating and speaking. They can arise from various causes, such as infections, injuries, autoimmune disorders, or underlying medical conditions. While some mouth lesions are harmless and resolve on their own, others may require medical attention, especially if they persist, worsen, or are accompanied by other symptoms like fever or swelling.
Canker Sores (Aphthous Ulcers): Canker sores are small, painful ulcers that appear inside the mouth, often on the inner cheeks, tongue, or gums. They are usually round or oval with a white or yellowish center and a red border. The exact cause is unknown, but factors like stress, minor mouth injuries, acidic foods, or nutritional deficiencies (such as vitamin B12 or iron) may trigger them. Oral canker lesions aren’t infectious and generally heal unaided within 10 to 14 days. Over-the-counter topical gels or mouth rinses can help relieve discomfort.
Cold Sores (Fever Blisters): Cold sores are fluid-filled blisters caused by the herpes simplex virus (HSV-1). They commonly appear on or around the lips but can also develop inside the mouth. These lesions are highly contagious and may recur due to triggers like stress, sunlight exposure, or illness. Initial outbreaks can be painful and may include flu-like symptoms. Antiviral medications can help reduce the severity and duration of outbreaks.
Oral Thrush (Candidiasis): Oral thrush is a fungal infection caused by Candida albicans, leading to creamy white lesions on the tongue, inner cheeks, or throat. It is more common in infants, the elderly, and individuals with weakened immune systems, diabetes, or those using antibiotics. Symptoms include a cottony feeling in the mouth, loss of taste, and mild bleeding if the lesions are scraped. Antifungal medications, such as nystatin or fluconazole, are typically used for treatment.
Leukoplakia: Leukoplakia presents as thick, white patches that cannot be scraped off and often form on the gums, tongue, or inner cheeks. It is usually caused by chronic irritation, such as tobacco use, rough teeth, or ill-fitting dentures. While most cases are benign, some may progress to oral cancer, so a biopsy is recommended for persistent lesions. Quitting tobacco and addressing irritants can help prevent leukoplakia.
Erythroplakia: Erythroplakia appears as red, velvety patches in the mouth and is less common but more concerning than leukoplakia, as it has a higher risk of being precancerous or cancerous. It often occurs on the floor of the mouth, tongue, or soft palate. A biopsy is essential for diagnosis, and surgical removal may be necessary if cancerous changes are detected.
Oral Lichen Planus: Oral lichen planus is an inflammatory condition that causes lacy white patches or red, swollen tissues in the mouth. The exact cause is unknown but may involve an autoimmune response. Symptoms can range from mild discomfort to severe pain, especially when eating spicy or acidic foods. Treatment may include corticosteroids or immune-modulating medications to manage symptoms.
Oral Cancer: Oral cancer lesions may appear as persistent ulcers, lumps, or discolored patches in the mouth that do not heal. Contributing factors encompass smoking, heavy drinking, and human papillomavirus exposure. Timely diagnosis is vital for effective care, which could entail surgical intervention, radiotherapy, or drug-based treatments. Routine oral exams aid in spotting abnormal growths at an earlier stage.
Each type of mouth lesion has distinct characteristics and potential health implications. Consulting a healthcare provider is important for proper diagnosis and treatment, especially if lesions persist, change in appearance, or cause significant discomfort.
Mouth lesions can present with a variety of symptoms and signs, depending on their underlying cause. These may include visible changes in the oral mucosa, discomfort, or systemic symptoms. Below is a detailed explanation of the common symptoms and signs associated with mouth lesions.
1. Pain or Discomfort: One of the most common symptoms of mouth lesions is pain or discomfort, which can range from mild irritation to severe, sharp pain. Pain may worsen when eating, drinking, or speaking, especially if the lesion is ulcerated or inflamed. Some conditions, such as canker sores (aphthous ulcers) or oral herpes, are particularly painful, while others, like leukoplakia, may be painless initially but become sore if irritated.
2. Visible Sores or Patches: Mouth lesions often appear as visible abnormalities on the gums, tongue, lips, cheeks, or palate. These may present as:
Ulcers: Shallow or deep open sores with a white or yellow center and red border (e.g., canker sores).
Blisters: Fluid-filled lesions, as seen in cold sores (herpes simplex virus) or hand, foot, and mouth disease.
White or Red Patches: Conditions like leukoplakia (white patches that cannot be scraped off) or erythroplakia (red patches) may indicate precancerous changes.
Lumps or Growths: These may be benign (e.g., fibromas) or malignant (oral cancer).
3. Swelling or Inflammation: Inflammation around the lesion may cause localized swelling, redness, or warmth. Infections, such as oral thrush (candidiasis) or bacterial abscesses, often lead to noticeable swelling. Allergic reactions or trauma (e.g., biting the cheek) can also result in swollen, tender areas.
4. Bleeding or Oozing: Some mouth lesions, particularly ulcers or growths, may bleed easily when touched or irritated. Bleeding can occur with traumatic ulcers, gingivitis, or oral cancer. Persistent bleeding without an obvious cause should be evaluated by a healthcare professional.
5. Difficulty Eating or Swallowing: Painful lesions or those located on the tongue, throat, or gums can interfere with chewing and swallowing. Conditions like oral lichen planus or severe aphthous stomatitis may make eating difficult, leading to dehydration or malnutrition if left untreated.
6. Bad Breath (Halitosis): Mouth lesions caused by infections (e.g., gingivostomatitis, periodontal disease) or necrotic tissue (as in some oral cancers) can produce a foul odor. Poor oral hygiene due to pain while brushing may also contribute to bad breath.
7. Numbness or Tingling: In rare cases, lesions associated with nerve involvement (such as oral cancer or herpes zoster) may cause numbness, tingling, or a burning sensation in the mouth or lips.
8. Systemic Symptoms: Some mouth lesions are linked to systemic conditions, leading to additional symptoms such as:
Fever: Seen in infections like herpetic gingivostomatitis or hand, foot, and mouth disease.
Swollen Lymph Nodes: Common with viral infections or oral cancers.
Skin Rashes: Conditions like lichen planus or autoimmune diseases (e.g., lupus, pemphigus vulgaris) may cause both oral and skin lesions.
While many mouth lesions heal on their own, persistent sores (lasting more than two weeks), rapidly growing lumps, or lesions accompanied by severe pain, bleeding, or systemic symptoms require medical evaluation. Early diagnosis is crucial, especially for potentially serious conditions like oral cancer or autoimmune disorders.
Mouth lesions are abnormal growths, ulcers, or sores that develop in the oral cavity, including the lips, tongue, gums, cheeks, and palate. These lesions can result from various causes, ranging from minor irritations to serious medical conditions. Understanding the underlying causes and risk factors can help in prevention, early diagnosis, and effective treatment.
Trauma or Injury
Physical trauma is one of the most common causes of mouth lesions. Accidental biting, sharp food edges, dental appliances (such as braces or dentures), and aggressive tooth brushing can damage the delicate tissues in the mouth, leading to ulcers or sores. Burns from hot food or beverages may also cause painful blisters or erosions.
Infections
Viral, bacterial, and fungal infections can lead to mouth lesions. Herpes simplex virus (HSV) causes cold sores or fever blisters, while the Coxsackievirus leads to hand, foot, and mouth disease, characterized by painful oral ulcers. Bacterial infections, such as syphilis or gonorrhea, may also produce oral lesions. Additionally, fungal infections like oral thrush (caused by Candida albicans) result in white, creamy patches inside the mouth.
Autoimmune Disorders
Certain autoimmune conditions trigger mouth lesions due to the body’s immune system attacking healthy tissues. Conditions like lichen planus cause white, lacy patches or red, swollen sores, while pemphigus vulgaris leads to painful blisters. Behçet’s disease, another autoimmune disorder, causes recurrent mouth ulcers along with other systemic symptoms.
Nutritional Deficiencies
A lack of essential vitamins and minerals, particularly vitamin B12, iron, folate, and zinc, can contribute to mouth ulcers. Deficiencies weaken the mucosal lining, making the mouth more susceptible to lesions. Poor nutrition also impairs the immune system, increasing the risk of infections that cause oral sores.
Allergic Reactions
Some individuals develop mouth lesions due to allergic reactions to certain foods (such as nuts, citrus, or spicy foods), medications, or dental products (like toothpaste or mouthwash containing sodium lauryl sulfate). These reactions may lead to canker sores or contact stomatitis, characterized by redness, swelling, and ulceration.
Chronic Diseases and Systemic Conditions
Systemic illnesses such as diabetes, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), and celiac disease are associated with mouth lesions. Poorly controlled diabetes increases the risk of oral thrush and slow-healing ulcers, while gastrointestinal disorders may cause nutritional deficiencies that lead to recurrent sores.
Poor Oral Hygiene
Inadequate brushing, flossing, and dental care allow harmful bacteria to accumulate, increasing the risk of infections and gum disease, which can lead to mouth sores.
Smoking and Alcohol Use
Tobacco and excessive alcohol consumption irritate the oral mucosa, increasing the likelihood of lesions, leukoplakia (white patches), and oral cancer.
Weakened Immune System
Individuals with HIV/AIDS, undergoing chemotherapy, or taking immunosuppressive drugs are more prone to infections like oral thrush and herpes-related mouth ulcers.
Hormonal Changes
Some women experience mouth ulcers during hormonal fluctuations, such as menstruation, pregnancy, or menopause, due to changes in immune response.
Genetic Predisposition
A family history of recurrent canker sores or autoimmune diseases may increase susceptibility to mouth lesions.
Stress and Anxiety
Emotional stress weakens the immune system and may trigger canker sores or exacerbate existing oral conditions.
By recognizing these causes and risk factors, individuals can take preventive measures, such as maintaining good oral hygiene, eating a balanced diet, and avoiding irritants, to reduce the likelihood of developing painful mouth lesions. If lesions persist or worsen, consulting a healthcare professional is essential for proper diagnosis and treatment.
The progression of mouth lesions depends on their type:
Early Stage – Mild irritation, redness, or small bumps appear.
Active Stage – Lesions become painful, may ulcerate, or develop white/red patches.
Healing Stage – Sores begin to shrink and pain subsides (for benign lesions).
Chronic/Advanced Stage – Persistent lesions that may indicate infection or malignancy (e.g., oral cancer).
Early detection is crucial, especially for lesions that could progress into serious conditions.
The diagnosis of mouth lesions involves a systematic approach to determine the underlying cause and guide appropriate treatment. Key steps include:
Clinical Evaluation
Medical History: Assessment of symptoms (pain, duration, recurrence), risk factors (tobacco/alcohol use, immunosuppression), and systemic conditions (diabetes, autoimmune diseases).
Physical Examination: Inspection of the lesion’s size, shape, color, texture, and location (tongue, gums, buccal mucosa). Palpation checks for tenderness, induration, or fixation to underlying tissues.
Diagnostic Tests
Biopsy (Punch, Incisional, or Excisional): Essential for suspicious or persistent lesions to rule out malignancy.
Imaging Studies (X-rays, CT, MRI): Used if bone involvement (osteomyelitis) or tumor spread is suspected.
Laboratory Tests: Blood tests (CBC, glucose, HIV/syphilis screening) for systemic causes; microbial cultures for infections (candidiasis, herpes).
Specialized Tests: Direct immunofluorescence for autoimmune conditions (e.g., pemphigus vulgaris).
Differential Diagnosis
Benign Lesions: Aphthous ulcers, fibromas, mucoceles.
Infectious: Herpes simplex, oral thrush, syphilitic chancres.
Premalignant/Malignant: Leukoplakia, erythroplakia, squamous cell carcinoma.
The prognosis varies widely based on etiology, early detection, and management. Key factors include:
Benign Lesions
Excellent Prognosis: Minor aphthous ulcers heal in 7–14 days; traumatic fibromas resolve post-excision.
Recurrent Conditions (e.g., herpes labialis): Manageable with antivirals but may recur during stress/immunosuppression.
Chronic/Inflammatory Conditions
Lichen Planus: Often chronic; 1–2% risk of malignant transformation requires long-term monitoring.
Autoimmune Disorders (e.g., pemphigus): Poor prognosis if untreated; corticosteroids/biologics improve outcomes.
Premalignant and Malignant Lesions
Leukoplakia/Erythroplakia: 5–18% risk of malignancy; excision and close follow-up are critical.
Oral Cancer:
Early-Stage (I–II): 5-year survival ~70–90% with surgery/radiation.
Advanced (III–IV): Drops to ~20–50%; lymph node involvement worsens prognosis.
Risk Factors: Tobacco/alcohol use, HPV status (HPV+ oropharyngeal cancer has better survival).
Lifestyle and Follow-Up
Smoking cessation, alcohol moderation, and oral hygiene reduce recurrence.
Regular dental visits for high-risk patients (e.g., history of oral cancer).
Mouth lesions can arise from various causes, including infections, trauma, autoimmune disorders, or systemic diseases. Treatment depends on the underlying cause, severity, and type of lesion. Below are the key approaches to managing mouth lesions:
Topical medications are often the first line of treatment for mild to moderate mouth lesions. These include:
Antimicrobial Mouthwashes (e.g., chlorhexidine gluconate) – Help reduce bacterial load and prevent secondary infections.
Topical Corticosteroids (e.g., triamcinolone acetonide, clobetasol) – Reduce inflammation in conditions like oral lichen planus or recurrent aphthous stomatitis.
Antifungal Gels or Lozenges (e.g., nystatin, clotrimazole) – Used for oral thrush (candidiasis).
Anesthetic Gels (e.g., lidocaine or benzocaine) – Provide temporary pain relief for ulcers or canker sores.
For severe or persistent lesions, systemic medications may be required:
Oral Antibiotics (e.g., amoxicillin, tetracycline) – Prescribed for bacterial infections causing mouth ulcers or abscesses.
Antiviral Drugs (e.g., acyclovir, valacyclovir) – Used for herpes simplex virus (HSV) infections like cold sores.
Immunosuppressants (e.g., prednisone, azathioprine) – Help manage autoimmune-related lesions such as pemphigus vulgaris.
Vitamin Supplements (e.g., B12, iron, folic acid) – Correct deficiencies that may contribute to recurrent mouth ulcers.
Pain relief is crucial for improving comfort, especially with ulcers or erosive lesions:
Over-the-counter (OTC) Pain Relievers – NSAIDs (ibuprofen) or acetaminophen can help reduce discomfort.
Topical Analgesics – Gels containing benzocaine or lidocaine numb the affected area.
Protective Pastes – Products like Orabase form a barrier over ulcers, reducing irritation from eating or drinking.
Supportive care can aid healing and prevent recurrence:
Oral Hygiene – Gentle brushing with a soft toothbrush and avoiding harsh mouthwashes with alcohol.
Dietary Adjustments – Avoiding spicy, acidic, or crunchy foods that may irritate lesions.
Hydration and Humidification – Drinking plenty of water and using a humidifier to prevent dry mouth.
Stress Management – Stress can trigger conditions like canker sores, so relaxation techniques may help.
In rare cases, medical procedures may be necessary:
Laser Therapy – Used for persistent ulcers or lesions like leukoplakia.
Cryotherapy – Freezing abnormal tissues (e.g., oral warts or precancerous lesions).
Biopsy and Excision – Required for suspicious lesions to rule out oral cancer.
Poor oral hygiene contributes to bacterial and fungal overgrowth, increasing the risk of lesions such as gingivitis, oral thrush, and periodontal disease. Patients should:
Brush teeth twice daily with a soft-bristled toothbrush to avoid gum irritation.
Use fluoride toothpaste to strengthen enamel and prevent decay.
Floss daily to remove plaque between teeth.
Rinse with an antiseptic mouthwash to reduce microbial load.
Tobacco and Alcohol: Both are major risk factors for oral cancer and leukoplakia. Smoking also impairs healing.
Spicy or Acidic Foods: These can trigger or worsen canker sores (aphthous ulcers).
Mechanical Trauma: Ill-fitting dentures, braces, or accidental biting can cause ulcers. Patients should ensure proper dental fittings and consider orthodontic wax for sharp edges.
Mouthguards: Athletes should wear them to prevent sports-related injuries.
Deficiencies in vitamin B12, iron, folate, and zinc are linked to recurrent mouth ulcers. A balanced diet rich in leafy greens, lean proteins, and whole grains helps prevent deficiencies. In some cases, supplements may be necessary.
Diabetes: Poor glycemic control increases infection risk (e.g., oral thrush).
Autoimmune Diseases: Conditions like lupus or Crohn’s disease may cause oral lesions; immunosuppressive therapy can help.
Herpes Simplex Virus (HSV): Antiviral drugs (e.g., acyclovir) can prevent recurrent cold sores.
Emotional stress is a known trigger for aphthous ulcers. Relaxation techniques (meditation, counseling) may reduce outbreaks.
Open sores can become infected with bacteria (e.g., Staphylococcus or Streptococcus), leading to:
Increased pain and swelling
Purulent discharge (pus)
Spread to surrounding tissues (cellulitis)
Ludwig’s angina (a life-threatening neck infection obstructing the airway)
Immunocompromised patients (e.g., HIV/AIDS, chemotherapy recipients) are at higher risk.
Persistent ulcers can make eating, drinking, and speaking painful, leading to:
Dehydration (due to reduced fluid intake)
Malnutrition and weight loss
Speech difficulties (if lesions affect the tongue or lips)
Some lesions have premalignant potential:
Leukoplakia (white patches): 3-5% risk of oral cancer.
Erythroplakia (red patches): Higher malignant potential.
Oral Lichen Planus: A small percentage may transform into squamous cell carcinoma.
Biopsy and regular monitoring are essential for suspicious lesions.
In rare cases, oral infections can enter the bloodstream, causing:
Sepsis (a life-threatening systemic infection)
Infective endocarditis (if bacteria infect heart valves)
Chronic mouth lesions may lead to:
Anxiety and depression (due to persistent pain or cosmetic concerns)
Social withdrawal (avoiding speaking or eating in public)
Mouth lesions can be a minor nuisance or a sign of a serious condition. Recognizing mouth lesions symptoms and signs, understanding their causes and risk factors, and seeking prompt diagnosis and treatment are key to maintaining oral health. By following prevention strategies, you can minimize risks and ensure early intervention if problems arise.
If you notice persistent or unusual changes in your mouth, consult a healthcare professional for proper evaluation. Your oral health is a vital part of your overall well-being—don’t ignore it!
Mouth lesions can result from various causes, including trauma (like biting your cheek or irritation from braces), infections (such as herpes simplex virus or oral thrush), canker sores, autoimmune conditions (like lupus or lichen planus), and nutritional deficiencies. Additionally, irritants like spicy foods, tobacco, or alcohol can trigger or worsen lesions.
A cancerous mouth lesion often appears as a persistent sore that doesn’t heal. It may look like a red or white patch, a lump, or an ulcer with raised edges. These lesions can occur on the tongue, inner cheeks, gums, or lips and are often painless at first. If a lesion lasts more than two weeks or starts to bleed or grow, it’s important to get it checked by a healthcare provider.
Treatment for mouth lesions depends on the cause. For minor irritations or canker sores, over-the-counter gels, saltwater rinses, and avoiding spicy or acidic foods can help. Antiviral or antifungal medications are used for infections, while steroid creams or rinses may be prescribed for autoimmune-related lesions. Maintaining good oral hygiene and managing any underlying conditions is also essential.
To get rid of oral lesions, identify and treat the underlying cause. Home remedies like saltwater rinses, baking soda pastes, and aloe vera gel can soothe irritation. For persistent or severe lesions, doctors may prescribe medication or recommend lifestyle changes such as quitting smoking or managing stress.
Yes, many mouth lesions heal on their own within a week or two, especially if they are due to minor trauma or canker sores. However, if they persist longer than 2–3 weeks, recur frequently, or are accompanied by other symptoms like pain or swelling, medical evaluation is necessary.
Deficiencies in several nutrients can lead to mouth lesions. Common culprits include iron, vitamin B12, folate, and vitamin C. For example, iron deficiency can cause painful sores, while vitamin C deficiency can lead to swollen, bleeding gums and ulcerations.
Fruits generally do not contain vitamin B12, as it is primarily found in animal products. However, some fortified foods like plant-based milks or cereals may include B12. For strict vegetarians or vegans, B12 supplements or fortified foods are often necessary.
Yes, stress is a known trigger for mouth lesions, particularly canker sores. Stress weakens the immune system, making the body more susceptible to inflammation and flare-ups of conditions like herpes simplex, which can cause cold sores.
Absolutely. A deficiency in vitamin B12 can lead to various oral symptoms, including painful ulcers, burning sensations in the mouth or tongue, and cracked lips. These symptoms often improve once B12 levels are restored through diet or supplements.
Vitamin B12 deficiency primarily affects the nervous system and the blood. It can lead to neurological issues like numbness, tingling, and memory problems, as well as anemia. The digestive tract, especially the stomach and intestines, may also be involved in cases where absorption is impaired.
Foods rich in vitamin B12 include animal-based products such as liver, beef, fish (like salmon and tuna), eggs, dairy products, and shellfish. For those on plant-based diets, fortified cereals, nutritional yeast, and B12 supplements are good options.
12. Can vitamin deficiency cause lesions?
Yes, several vitamin deficiencies can cause or worsen mouth lesions. In particular, deficiencies in B vitamins (B1, B2, B6, B12), folate, iron, and vitamin C are linked to oral sores, inflammation, and delayed healing. A balanced diet is key to preventing these issues.