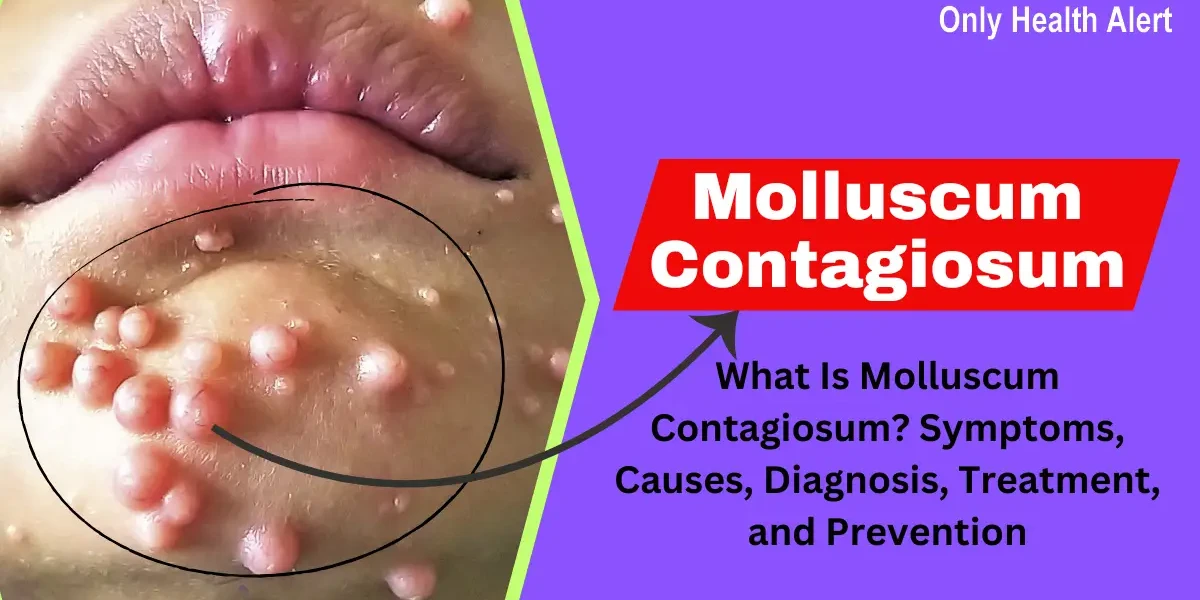
Molluscum contagiosum is a common, yet often misunderstood, viral skin infection that causes small, raised bumps on the skin. While it’s usually harmless and resolves on its own, it can be bothersome, especially for children, sexually active adults, and people with weakened immune systems.
In this comprehensive guide, we’ll explore everything you need to know about molluscum contagiosum, including its symptoms, causes, diagnosis, treatment options, and prevention strategies. Whether you're a concerned parent, a patient, or just curious, this article will provide clear, expert-backed insights.
What Is Molluscum Contagiosum?
Molluscum contagiosum is a viral skin infection caused by the molluscum contagiosum virus (MCV), a member of the poxvirus family. The infection leads to the development of small, flesh-colored, or pearly bumps (called mollusca) that often have a dimple in the center. These bumps are typically painless but can become itchy, red, or inflamed.
The virus spreads through direct skin-to-skin contact or by touching contaminated objects, such as towels, toys, or gym equipment. While it can affect anyone, it’s most common in:
Types of Molluscum Contagiosum
Molluscum contagiosum is a viral skin infection caused by the Molluscum contagiosum virus (MCV), primarily affecting children, sexually active adults, and immunocompromised individuals. The condition presents as small, flesh-colored, dome-shaped bumps with a central dimple. While there are no formally classified "types" of molluscum contagiosum, the lesions can vary in appearance, distribution, and severity based on the host's immune status and the mode of transmission. Below are the key clinical variations:
1. Classic Molluscum Contagiosum (Localized Skin Lesions)
The most common presentation consists of small (2–5 mm), pearly, umbilicated papules that appear on the skin. These lesions often occur in clusters and are typically found in areas where skin-to-skin contact is frequent, such as the face, neck, armpits, arms, and hands in children. In sexually active adults, they may appear on the lower abdomen, inner thighs, and genital region. The lesions are usually painless but can become inflamed or itchy if scratched or infected. Classic molluscum contagiosum is self-limiting in immunocompetent individuals, resolving within 6–12 months without scarring.
2. Giant Molluscum Contagiosum (Large or Coalescing Lesions)
Some individuals develop larger lesions (greater than 5 mm), known as giant molluscum contagiosum. These occur due to the fusion of multiple smaller lesions or an exaggerated local immune response. Giant molluscum is more common in immunocompromised patients, such as those with HIV/AIDS or undergoing immunosuppressive therapy. These lesions may persist for years and can be more challenging to treat, sometimes requiring surgical removal or laser therapy.
3. Disseminated Molluscum Contagiosum (Widespread Infection)
In immunocompromised individuals (e.g., HIV patients or organ transplant recipients), molluscum contagiosum can spread extensively across the body, with hundreds of lesions covering large areas, including the face and trunk. Unlike the localized form, these lesions may not resolve spontaneously and often require systemic or aggressive treatments such as antiviral therapy, immunotherapy, or highly active antiretroviral therapy (HAART) in HIV patients.
4. Eczema-Associated Molluscum Contagiosum (Molluscum Dermatitis)
Some patients with pre-existing eczema (atopic dermatitis) may develop a more severe inflammatory reaction around molluscum lesions, leading to redness, swelling, and intense itching. This condition, known as molluscum dermatitis, can worsen eczema symptoms and increase the risk of secondary bacterial infections. Managing both the molluscum and underlying eczema is essential to prevent complications.
5. Follicular Molluscum Contagiosum (Hair Follicle Involvement)
In rare cases, molluscum lesions can develop within hair follicles, appearing as grouped papules with central hairs. This variant may mimic folliculitis or other hair follicle disorders, requiring careful diagnosis.
While molluscum contagiosum is generally harmless, the type and extent of lesions depend on the patient's immune status. Treatment options range from watchful waiting in mild cases to cryotherapy, curettage, topical agents (e.g., podophyllotoxin or imiquimod), and systemic therapies in severe or persistent infections.
Molluscum Contagiosum Symptoms and Signs
Molluscum contagiosum is a viral skin infection characterized by distinctive, benign growths that appear on the skin’s surface. Caused by the Molluscum contagiosum virus (MCV), this condition is highly contagious and spreads through direct skin-to-skin contact, shared towels or clothing, and sexual contact. While it is most frequently seen in children between the ages of 1 and 10, it can also affect sexually active adults and individuals with weakened immune systems. The hallmark of this infection is the development of small, raised bumps that are typically flesh-colored, pink, or pearly white. These lesions are usually smooth and firm, with a central indentation (umbilication) that gives them a unique appearance under close examination.
Primary Symptoms and Clinical Presentation
The most recognizable sign of molluscum contagiosum is the presence of round, dome-shaped papules ranging from 2 to 5 millimeters in diameter, though they can occasionally grow larger, particularly in immunocompromised individuals. The lesions often start as tiny, pinhead-sized spots that gradually enlarge over several weeks. Upon maturation, they develop a waxy or pearly sheen, and the central dimple becomes more pronounced. This umbilication is a key diagnostic feature, helping to distinguish molluscum from other skin conditions like warts, herpes, or folliculitis. When the lesions are squeezed, a thick, white, cheesy material (composed of viral particles and dead skin cells) may be expressed, though this is not recommended as it can spread the infection.
The distribution of molluscum lesions varies depending on the mode of transmission:
Secondary Symptoms and Complications
While molluscum contagiosum is generally harmless and painless, some patients experience secondary symptoms due to irritation or immune response:
Special Considerations in High-Risk Groups
1. Children: Young children are particularly susceptible due to their close physical contact in schools and daycare settings. The lesions often appear on the face, arms, and hands, which can lead to social embarrassment or concern from parents. Since children may scratch or pick at the bumps, keeping the area clean and covered can help prevent spread.
2. Sexually Active Adults: In adults, molluscum contagiosum is often considered a sexually transmitted infection (STI) when lesions appear in the genital area. Unlike herpes or HPV, molluscum does not cause ulcers or increase cancer risk, but its presence may warrant screening for other STIs. Sexual partners should also be examined, as the virus can be transmitted even with condom use (since condoms do not cover all affected skin).
3. Immunocompromised Individuals: Patients with HIV/AIDS, chemotherapy recipients, or those on long-term corticosteroids may experience "giant molluscum" (lesions larger than 1 cm) or disseminated infections with hundreds of bumps. These cases often require medical intervention, as spontaneous resolution is unlikely without immune reconstitution.
When to Seek Medical Attention
While molluscum contagiosum typically resolves on its own, medical evaluation is recommended if:
Molluscum Contagiosum Causes and Risk Factors
1. Viral Origin and Transmission
Molluscum contagiosum is caused by the molluscum contagiosum virus (MCV), a DNA virus from the Poxviridae family, which also includes viruses like smallpox and monkeypox. Unlike some other viruses, MCV only infects humans and cannot be transmitted from animals. There are four main subtypes of MCV (MCV-1 to MCV-4), with MCV-1 being the most common, especially in children, while MCV-2 is more frequently seen in adults and immunocompromised patients.
Modes of Transmission
The virus spreads through several mechanisms:
2. Risk Factors for Molluscum Contagiosum
A. Age and Close-Contact Settings
B. Weakened Immune System
C. Skin Conditions
D. Environmental and Hygiene Factors
3. Why Some People Get Severe Infections
While most healthy individuals develop only a few lesions that resolve within 6-12 months, certain factors lead to prolonged or severe infections:
4. Prevention Strategies
Molluscum Contagiosum Stages
Molluscum contagiosum is a common viral skin infection caused by the Molluscum contagiosum virus (MCV), a member of the poxvirus family. The infection progresses through several stages, from initial exposure to resolution. Understanding these stages helps in identifying the condition and managing it effectively.
1. Incubation Period (Exposure to First Signs)
After exposure to the virus, there is an incubation period that typically lasts between 2 to 7 weeks, though it can extend up to 6 months in some cases. During this stage, the virus multiplies within the skin cells, but no visible symptoms appear. The infection spreads through direct skin-to-skin contact, sharing contaminated items (like towels or clothing), or sexual contact in adults. Since there are no symptoms at this stage, individuals may unknowingly transmit the virus to others.
2. Appearance of Lesions (Early Stage)
The first visible sign of molluscum contagiosum is the appearance of small, flesh-colored, pink, or pearly white bumps (papules) on the skin. These lesions are usually 2–5 mm in diameter but can grow larger in immunocompromised individuals. They often have a central dimple or indentation and a waxy or shiny appearance. The bumps may appear singly or in clusters and commonly affect areas such as the face, neck, armpits, arms, hands, and genital region (if transmitted sexually). At this stage, the lesions are typically painless but may become itchy or irritated if scratched.
3. Growth and Spread (Active Stage)
Over the following weeks, the lesions may increase in size and number as the virus continues to replicate. Scratching or rubbing the bumps can lead to auto-inoculation, where the infection spreads to nearby skin. The lesions remain contagious throughout this stage, and contact with them can transmit the virus to others. In healthy individuals, the immune system gradually begins to recognize and fight the infection, but this process can take time. Some lesions may become inflamed, red, or sore, especially if secondary bacterial infections occur due to scratching.
4. Resolution and Healing (Final Stage)
In most cases, molluscum contagiosum resolves on its own within 6 to 12 months, though some cases may persist for several years, particularly in people with weakened immune systems. As the immune system clears the virus, the lesions may become red, inflamed, or crusted before eventually drying up and disappearing. Scarring is rare, but some lesions may leave temporary light or dark marks (post-inflammatory hyperpigmentation or hypopigmentation) that fade over time. Once all lesions have healed, the virus is no longer contagious, and reinfection is possible only upon new exposure.
Molluscum Contagiosum Diagnosis
1. Clinical Examination
Molluscum contagiosum is primarily diagnosed through a clinical examination by a healthcare provider. The characteristic lesions are small, firm, dome-shaped, and pearly or flesh-colored with a central dimple (umbilication). They typically range from 2 to 5 millimeters in diameter but can grow larger in immunocompromised individuals. The bumps often appear in clusters on the face, trunk, arms, legs, or genital area in adults. Since the lesions have a distinct appearance, a visual inspection is usually sufficient for diagnosis. However, if the presentation is atypical, further diagnostic tests may be required.
2. Dermoscopy
Dermoscopy, a non-invasive skin imaging technique, can aid in the diagnosis of molluscum contagiosum. Under dermoscopic examination, the lesions show a polylobular, white-to-yellow amorphous structure with surrounding crown-like blood vessels. The central umbilication, which is a hallmark feature, is often more clearly visible under dermoscopy. This method helps differentiate molluscum contagiosum from other skin conditions such as warts, skin tags, or basal cell carcinoma, which may have similar appearances to the naked eye.
3. Skin Biopsy and Histopathology
In rare cases where the diagnosis is uncertain, a skin biopsy may be performed. A small sample of the lesion is examined under a microscope, revealing characteristic intracytoplasmic inclusion bodies called molluscum bodies or Henderson-Paterson bodies within the infected cells. Histopathology confirms the presence of the molluscum contagiosum virus (MCV), a member of the poxvirus family. This method is particularly useful in immunocompromised patients who may have atypical or widespread lesions that resemble other skin disorders.
4. Polymerase Chain Reaction (PCR) Testing
PCR testing can detect molluscum contagiosum virus DNA in lesion samples, providing a definitive diagnosis. This method is highly sensitive and specific, making it useful in research settings or for cases where clinical and histopathological findings are inconclusive. However, due to its cost and limited necessity in typical cases, PCR is not routinely used for diagnosis unless other conditions, such as herpes or atypical infections, need to be ruled out.
5. Differential Diagnosis
Since molluscum contagiosum can resemble other skin conditions, healthcare providers must consider differential diagnoses. Common mimics include warts (caused by HPV), herpes simplex virus (HSV) lesions, folliculitis, basal cell carcinoma, and keratoacanthoma. The absence of pain (unless secondary infection occurs) and the presence of central umbilication help distinguish molluscum contagiosum from these conditions. In sexually active adults with genital lesions, testing for other sexually transmitted infections (STIs) may also be recommended.
Prognosis of Molluscum Contagiosum
The prognosis is generally excellent for healthy individuals:
Scarring is rare unless lesions are scratched or improperly treated.
Molluscum Contagiosum Treatment and Medication
Since molluscum contagiosum is a benign condition, treatment is not always necessary. However, when required, options include physical removal, topical medications, oral medications, and immune-modulating therapies. The choice of treatment depends on the patient’s age, immune status, lesion location, and severity.
1. Physical Removal Methods
These procedures are performed by a healthcare provider and are effective for immediate lesion clearance:
2. Topical Medications
These are applied directly to lesions and work by inducing inflammation, triggering an immune response, or directly destroying the virus:
3. Oral Medications
Used in severe or resistant cases, particularly in immunocompromised patients:
4. Immune-Based Therapies
For patients with weakened immune systems (e.g., HIV/AIDS), stronger treatments may be needed:
Choosing the Right Treatment
Prevention of Molluscum Contagiosum
Molluscum contagiosum is a viral skin infection caused by the Molluscum contagiosum virus (MCV). It spreads through direct skin-to-skin contact, contaminated objects, or sexual contact. While the infection is usually harmless and resolves on its own, preventing its spread is important, especially among children, athletes, and sexually active individuals. Below are detailed preventive measures:
1. Practice Good Personal Hygiene: Maintaining proper hygiene is essential in preventing the spread of molluscum contagiosum. Regular handwashing with soap and water helps eliminate the virus from the skin, especially after touching infected areas. Since the virus can survive on surfaces, avoiding touching the bumps and then touching other body parts reduces self-inoculation. Additionally, individuals with the infection should avoid sharing personal items like towels, razors, or clothing to prevent transmission to others.
2. Avoid Direct Skin-to-Skin Contact: Since molluscum contagiosum spreads through direct contact, avoiding close physical contact with infected individuals is crucial. This is particularly important in settings like schools, gyms, and swimming pools, where skin exposure is common. Parents should monitor children with molluscum and cover their bumps with waterproof bandages to minimize transmission during play. Similarly, athletes involved in contact sports (e.g., wrestling) should cover lesions and avoid sharing sports gear.
3. Refrain from Scratching or Picking at Bumps: Scratching or shaving over molluscum bumps can spread the virus to other parts of the body (autoinoculation). To prevent this, individuals should keep the affected areas clean and covered with clothing or bandages. If itching occurs, applying an over-the-counter anti-itch cream or consulting a doctor for proper treatment can help avoid further irritation and spreading.
4. Disinfect Shared Surfaces and Objects: The virus can survive on surfaces such as gym equipment, towels, and toys. Regularly disinfecting these items with antiviral solutions (e.g., bleach-based cleaners or alcohol-based sanitizers) reduces the risk of transmission. In households with an infected person, washing bedding, clothing, and towels in hot water can help kill the virus.
5. Practice Safe Sexual Habits: Molluscum contagiosum can spread through sexual contact when lesions are present in the genital area. Using condoms may reduce transmission but does not provide complete protection since the virus can spread through skin contact outside the covered area. Individuals with genital molluscum should abstain from sexual activity until the lesions are fully healed to prevent infecting their partners.
6. Keep Skin Dry and Avoid Moist Environments: The virus thrives in warm, moist environments, making swimming pools, locker rooms, and humid climates potential hotspots for transmission. Drying the skin thoroughly after bathing or swimming and avoiding prolonged exposure to damp conditions can help prevent infection. People with molluscum should avoid public pools until their lesions have cleared to prevent spreading the virus to others.
By following these preventive measures, individuals can reduce the risk of contracting and spreading molluscum contagiosum. While the infection is generally mild, taking precautions helps protect vulnerable populations, including young children and immunocompromised individuals, from prolonged or severe cases. If an infection persists or spreads extensively, consulting a healthcare provider for treatment options is recommended.
Complications of Molluscum Contagiosum
Molluscum contagiosum is generally a mild and self-limiting viral skin infection, but in some cases, it can lead to complications—particularly in certain high-risk groups, such as young children, individuals with eczema, or immunocompromised patients. While most people experience only minor skin lesions that resolve on their own, complications can arise from secondary infections, extensive spread, or delayed healing. Below, we discuss the potential complications in detail.
1. Secondary Bacterial Infections
One of the most common complications of molluscum contagiosum is a secondary bacterial infection, usually caused by Staphylococcus aureus or Streptococcus pyogenes. This occurs when the lesions are scratched, picked, or irritated, breaking the skin barrier and allowing bacteria to invade. Signs of a bacterial infection include increased redness, warmth, swelling, pain, and pus discharge. In severe cases, cellulitis (a deeper skin infection) or abscess formation may occur, requiring antibiotic treatment—either topical (e.g., mupirocin) or oral (e.g., cephalexin). Children with eczema are particularly prone to this complication because their skin barrier is already compromised. Keeping the skin clean, avoiding scratching, and using antiseptic washes can help prevent secondary infections.
2. Widespread or Persistent Lesions (Giant Molluscum)
In healthy individuals, molluscum contagiosum lesions typically resolve within 6–12 months. However, in people with weakened immune systems—such as those with HIV/AIDS, undergoing chemotherapy, or taking immunosuppressive drugs—the infection can become widespread, persistent, and difficult to treat. These patients may develop "giant molluscum", where lesions grow larger than 1 cm and appear in clusters. Unlike typical molluscum, these lesions may not resolve without aggressive treatment, such as cryotherapy, laser therapy, or systemic antivirals. Immunocompromised individuals may also experience recurrent outbreaks even after initial clearance, requiring long-term dermatologic management.
3. Eczema Flare-Ups (Molluscum Dermatitis)
Patients with pre-existing eczema (atopic dermatitis) are at higher risk for molluscum-associated dermatitis, where the skin around the molluscum lesions becomes inflamed, red, and intensely itchy. This occurs due to an immune reaction to the virus, exacerbating the underlying eczema. The resulting itch-scratch cycle can lead to further spread of molluscum and increase the risk of secondary infections. Managing this complication involves treating both the molluscum (e.g., with cantharidin or curettage) and the eczema (with moisturizers and topical steroids). In some cases, calcineurin inhibitors like tacrolimus may be used to reduce inflammation without thinning the skin.
4. Scarring and Skin Discoloration
While molluscum contagiosum lesions usually heal without scarring, complications can arise from aggressive scratching or improper treatment. Picking or squeezing the lesions can lead to post-inflammatory hyperpigmentation (dark spots) or hypopigmentation (light spots), especially in darker skin tones. Additionally, some treatment methods—such as cryotherapy, curettage, or laser therapy—may cause temporary scarring if not performed carefully. To minimize this risk, gentle treatment options (e.g., topical retinoids or immune modulators) may be preferred in cosmetically sensitive areas like the face.
5. Eye Complications (Conjunctivitis or Keratitis)
When molluscum lesions appear near the eye—particularly on the eyelids—they can lead to viral conjunctivitis (pink eye) or keratitis (corneal inflammation). This happens when viral particles from the lesions come into contact with the eye, causing redness, irritation, and discharge. In rare cases, chronic irritation can lead to corneal abrasions or secondary bacterial eye infections. Patients with periocular molluscum should avoid rubbing their eyes and seek treatment (such as lesion removal by curettage or cryotherapy) to prevent ocular complications. An ophthalmologist may be consulted if eye symptoms develop.
6. Psychological and Social Impact
Although not a physical complication, molluscum contagiosum can cause significant emotional distress, especially in children and sexually active adults. Parents may worry about their child being stigmatized at school or swimming pools due to visible lesions. Adults with genital molluscum may experience embarrassment, anxiety, or relationship strain due to the misconception that it is a sexually transmitted infection (STI). Counseling and education about the benign nature of molluscum can help alleviate concerns, and early treatment may be recommended to reduce social discomfort.
Conclusion
While molluscum contagiosum is usually harmless, complications can occur, particularly in high-risk individuals. Secondary infections, persistent lesions, eczema flare-ups, scarring, eye involvement, and psychological distress are the main concerns. Proper skin care, avoiding manipulation of lesions, and timely medical intervention can help prevent and manage these complications. Immunocompromised patients or those with severe cases should seek dermatologic care to minimize long-term effects.
FAQ's
Molluscum contagiosum is caused by the molluscum contagiosum virus (MCV), a member of the poxvirus family. The infection spreads through direct skin-to-skin contact, contact with contaminated objects (like towels or toys), or sexual contact in adults. It commonly affects children, athletes in close-contact sports, and individuals with weakened immune systems.
In many cases, molluscum resolves on its own within 6–12 months without treatment. However, if removal is desired, options include:
Cryotherapy (freezing)
Curettage (scraping off lesions)
Topical treatments (e.g., imiquimod, tretinoin, cantharidin)
Laser therapy
Natural immune response support (keeping skin clean and avoiding scratching)
Treatment choice depends on the patient’s age, immune status, and lesion location.
Molluscum contagiosum can be sexually transmitted if lesions are in the genital area, but it is not exclusively an STD. In children, it spreads through non-sexual skin contact or shared items. In adults with genital lesions, it may be considered an STI (sexually transmitted infection).
Yes, molluscum contagiosum usually clears up on its own within 6–18 months as the immune system fights the virus. However, in immunocompromised individuals, it may persist longer and require medical treatment.
The final stage involves lesions becoming inflamed, red, and crusty before drying out and disappearing. This indicates the immune system is attacking the virus. Scarring is rare but may occur if lesions are scratched or picked.
Skin bumps can result from:
Infections (molluscum, warts, folliculitis)
Allergic reactions (hives, eczema)
Blocked pores (acne, keratosis pilaris)
Autoimmune conditions (psoriasis, lichen planus)
Cysts or lipomas (benign growths)
Treatment depends on the cause:
Topical creams (retinoids, antibiotics, antifungals)
Cryotherapy or laser removal
Dermatologist extraction (for cysts, milia)
Oral medications (for severe acne or infections)
Home care (warm compresses, exfoliation)
Consult a doctor if a lump:
Grows rapidly
Is painful or hard
Doesn’t move under the skin
Is accompanied by fever or night sweats
Changes color or bleeds
These could indicate cysts, abscesses, or tumors (rarely cancerous).
Common skin conditions include:
Acne
Eczema (atopic dermatitis)
Psoriasis
Rosacea
Dermatitis (contact/allergic)
Fungal infections (ringworm, athlete’s foot)
Vitiligo
Cold sores (herpes simplex)
Warts (HPV)
Skin cancer (melanoma, basal cell carcinoma)
Doctors may order:
Complete Blood Count (CBC) (checks for infection)
C-reactive protein (CRP) or ESR (inflammation markers)
Culture tests (for bacterial/fungal infections)
HIV or autoimmune panels (if recurrent infections)
Eczema is not curable but manageable. Treatments include:
Moisturizers & steroid creams
Antihistamines (for itching)
Immunosuppressants (for severe cases)
Lifestyle changes (avoiding triggers like allergens)
Seek medical help if the rash:
Covers large areas
Is accompanied by fever or lethargy
Shows signs of infection (pus, swelling)
Causes difficulty breathing (allergic reaction)
Doesn’t improve in a few days
Common causes include eczema, viral infections (chickenpox), or allergies.
You Might Also Like