Migraine is more than just a headache—it’s a complex neurological condition that affects millions of people worldwide. Characterized by intense, throbbing pain, often on one side of the head, migraines can be debilitating, disrupting daily life and productivity. But what exactly causes them? How are they diagnosed and treated? And most importantly, can they be prevented?
A migraine is a neurological disorder that causes severe, recurrent headaches, often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Unlike regular tension headaches, migraines can last for hours or even days, significantly impairing a person’s ability to function.
According to the World Health Organization (WHO), migraines are among the top 10 most disabling medical illnesses globally, affecting about 1 in 7 people. Women are three times more likely to experience migraines than men, likely due to hormonal influences.
Migraine is a neurological condition characterized by intense, throbbing headaches, often accompanied by nausea, vomiting, and sensitivity to light and sound. There are several types of migraines, each with distinct symptoms and triggers. Understanding these types can help in proper diagnosis and treatment.
Migraine without aura is the most prevalent type, affecting about 70-90% of migraine sufferers. This type involves moderate to severe headache pain, typically on one side of the head, which worsens with physical activity. Symptoms include nausea, vomiting, and extreme sensitivity to light (photophobia) and sound (phonophobia). Unlike migraine with aura, this type does not involve visual or sensory disturbances before the headache begins. Triggers can include stress, hormonal changes, certain foods, lack of sleep, and environmental factors.
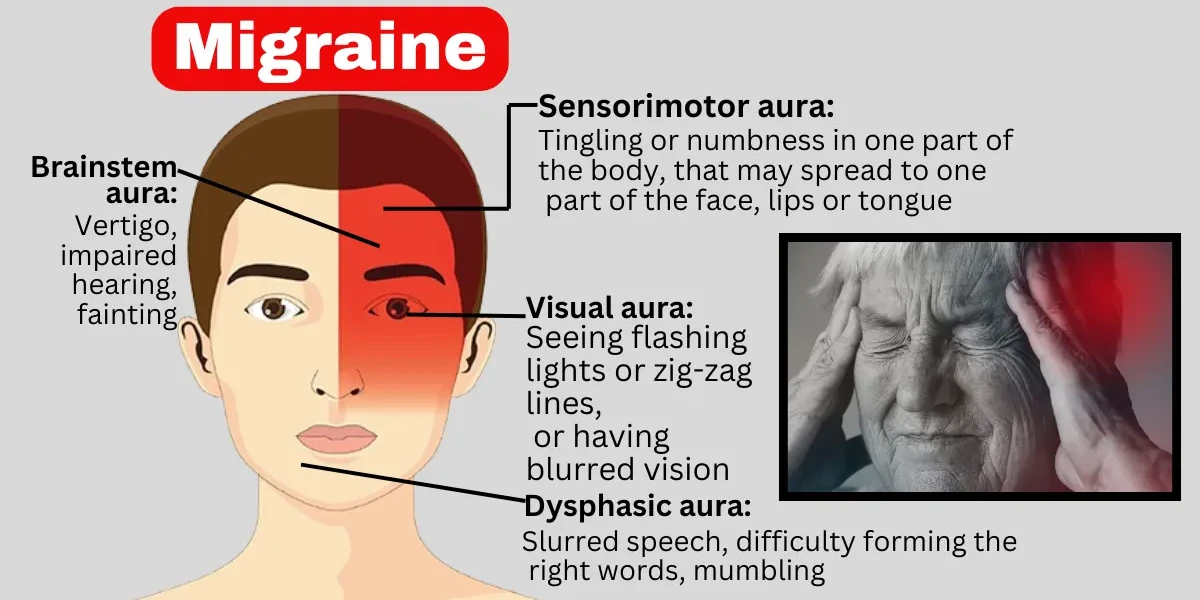
About 25-30% of migraine patients experience aura—a series of neurological symptoms that occur before or during the headache. Aura symptoms may include visual disturbances (flashing lights, zigzag patterns, blind spots), tingling sensations in the face or hands, speech difficulties, and even temporary vision loss. These symptoms usually last between 20 minutes to an hour and are followed by a severe headache. Some people may experience aura without a subsequent headache, known as "silent migraine."
Chronic migraine is diagnosed when a person experiences headaches on 15 or more days per month for at least three months, with at least eight of those headaches being migraines. This condition can significantly impact daily life, leading to disability and reduced quality of life. Chronic migraine often develops from episodic migraines that increase in frequency over time. Risk factors include overuse of pain medications, high stress levels, obesity, and sleep disorders.
Hemiplegic migraine is a rare and severe subtype that causes temporary weakness or paralysis on one side of the body (hemiplegia), resembling a stroke. Other symptoms may include vision problems, difficulty speaking, confusion, and loss of coordination. These episodes can last from a few hours to several days. There are two forms: familial hemiplegic migraine (inherited) and sporadic hemiplegic migraine (no family history). Due to its severity, proper medical evaluation is essential to rule out other neurological conditions.
Retinal migraine is characterized by temporary vision loss or visual disturbances in one eye, such as flashing lights or blind spots, lasting from minutes to an hour. Unlike aura-related visual symptoms, which affect both eyes, retinal migraine symptoms are restricted to one eye. This type is rare but can be alarming, and in some cases, it may indicate a more serious underlying condition, requiring medical attention.
Vestibular migraine primarily affects balance and causes dizziness, vertigo, and disorientation, with or without a headache. People with this type may experience motion sensitivity, nausea, and difficulty concentrating. It is often misdiagnosed as inner ear disorders like Ménière’s disease. Triggers include stress, lack of sleep, certain foods, and hormonal fluctuations.
Hormonal fluctuations, particularly drops in estrogen levels before or during menstruation, can trigger menstrual migraines. These migraines typically occur in the days leading up to or during a woman’s period and may be more severe and longer-lasting than regular migraines. Some women experience migraines only during menstruation (pure menstrual migraine), while others have them at other times as well (menstrually related migraine).
Status migrainosus is a severe and debilitating migraine attack that lasts for more than 72 hours, often resistant to standard treatments. The pain and accompanying symptoms (nausea, vomiting, dehydration) can be so intense that hospitalization may be required for intravenous medications and fluids. This condition can be triggered by medication overuse, abrupt withdrawal from certain drugs, or extreme stress.
Understanding the different types of migraines helps in identifying triggers, seeking appropriate treatment, and improving management strategies. If migraines are frequent or severe, consulting a healthcare provider is essential for proper diagnosis and personalized care.
Migraines are more than just headaches—they are a complex neurological condition with a variety of symptoms that can vary from person to person. The most common signs include throbbing head pain, nausea, sensitivity to light and sound, and visual disturbances. These symptoms can last for hours or even days, significantly impacting daily life.
1. Throbbing or Pulsating Head Pain: One of the hallmark symptoms of a migraine is intense, throbbing pain, usually on one side of the head (though it can affect both sides). The pain often worsens with physical activity and can be severe enough to interfere with work, school, or other routine activities. Unlike a regular tension headache, migraine pain tends to be more debilitating and may not respond well to standard pain relievers.
2. Nausea and Vomiting: Many migraine sufferers experience nausea, sometimes leading to vomiting. This symptom is thought to be linked to the way migraines affect the nervous system, particularly the brainstem and gut-brain connection. The nausea can make it difficult to eat or drink, further complicating recovery.
3. Sensitivity to Light (Photophobia) and Sound (Phonophobia): During a migraine attack, bright lights, screens, or even normal indoor lighting can feel unbearable. Similarly, everyday sounds—such as conversations, traffic, or music—may become intolerable. This heightened sensitivity is due to abnormal processing of sensory information in the brain during a migraine.
4. Visual Disturbances (Aura): About 25-30% of migraine sufferers experience aura, a neurological phenomenon that typically occurs before the headache phase. Aura symptoms may include flashing lights, zigzag patterns, blind spots, or temporary vision loss. Some people also experience tingling in the face or hands, difficulty speaking, or even temporary paralysis (hemiplegic migraine).
5. Dizziness and Vertigo: Some individuals with migraines experience dizziness, a spinning sensation (vertigo), or balance problems. This is more common in vestibular migraines, where the attack affects the inner ear and balance centers in the brain.
6. Fatigue and Cognitive Difficulties (Brain Fog): After a migraine attack, many people feel extremely tired and mentally drained. This "postdrome" phase, sometimes called a "migraine hangover," can involve difficulty concentrating, mood changes, and general weakness.
7. Neck Pain and Stiffness: Neck stiffness or pain is a common migraine symptom, either before or during an attack. Some researchers believe this is due to shared nerve pathways between the neck and head, or tension in the muscles triggered by the migraine.
Some people also experience prodrome symptoms (early warning signs) a day or two before the headache, such as:
Mood changes (irritability, depression, or euphoria)
Food cravings
Frequent yawning
Fatigue
Migraines represent a intricate neurological disorder marked by severe, pulsating head pain, frequently paired with nausea, vomiting, and heightened sensitivity to light and noise. While the exact cause of migraines is not fully understood, research suggests that a combination of genetic, environmental, and neurological factors contribute to their development.
1. Genetic Predisposition: A strong genetic link exists in migraines, particularly in cases of familial hemiplegic migraine (FHM), a rare subtype. If one or both parents suffer from migraines, their children have a significantly higher likelihood of developing them. Specific gene mutations, such as those affecting ion channels and neurotransmitter regulation in the brain (e.g., CACNA1A, ATP1A2, and SCN1A genes), have been identified in migraine sufferers. These genetic abnormalities may lead to hyperexcitability of neurons, making the brain more susceptible to migraine triggers.
2. Neurological and Vascular Factors: Migraines were once thought to be caused by blood vessel dilation, but current research highlights abnormal brain activity as the primary driver. The trigeminovascular system, which involves the trigeminal nerve (the largest cranial nerve), plays a key role. When activated, this nerve releases inflammatory neuropeptides (such as calcitonin gene-related peptide, or CGRP), causing blood vessels to dilate and triggering pain signals. Additionally, cortical spreading depression (CSD), a wave of electrical silence followed by hyperactivity in the brain, is believed to be responsible for migraine aura—a phenomenon where patients experience visual disturbances, tingling, or speech difficulties before the headache phase.
3. Neurochemical Imbalances: Serotonin, a neurotransmitter that regulates mood, pain, and sleep, fluctuates abnormally during migraines. A sudden drop in serotonin levels may lead to blood vessel changes and inflammation, contributing to migraine pain. Other neurotransmitters, such as dopamine and glutamate, also play a role in migraine susceptibility. Medications like triptans work by stabilizing serotonin levels and constricting blood vessels, providing relief.
1. Gender and Hormonal Influences: Women are three times more likely than men to suffer from migraines, largely due to hormonal fluctuations. Estrogen, in particular, influences migraine occurrence—many women experience migraines around menstruation (menstrual migraines), during ovulation, or in perimenopause. The drop in estrogen levels just before menstruation is a well-known trigger. Hormonal contraceptives and hormone replacement therapy (HRT) can either worsen or improve migraines, depending on the individual.
2. Age and Life Stages: Migraines often begin in adolescence or early adulthood, peaking in the 30s and 40s, and may decrease in frequency with age. Some women experience relief after menopause, while others develop migraines for the first time during this transition. Children can also suffer from migraines, often presenting as abdominal pain or dizziness rather than severe headaches.
3. Lifestyle and Environmental Triggers: Several external factors can provoke migraines in susceptible individuals:
Dietary Triggers: Aged cheeses (tyramine), processed meats (nitrates), alcohol (especially red wine), caffeine (withdrawal can trigger migraines), artificial sweeteners (aspartame), and MSG.
Sleep Disturbances: Both insufficient sleep and oversleeping can trigger migraines. Maintaining a regular sleep schedule is crucial.
Stress and Anxiety: Emotional stress leads to the release of cortisol and adrenaline, which may contribute to migraine attacks.
Sensory Stimuli: Bright lights (photophobia), loud noises (phonophobia), strong smells (perfumes, smoke), and even weather changes (barometric pressure shifts) can act as triggers.
Physical Factors: Intense exercise, poor posture, and jaw clenching (TMJ disorders) can contribute to tension that evolves into migraines.
4. Comorbid Medical Conditions
Certain health conditions increase migraine risk:
Depression and Anxiety: These disorders share a bidirectional relationship with migraines—each can worsen the other.
Hypertension and Cardiovascular Disease: Poor blood flow and vascular health may contribute to migraine frequency.
Epilepsy and Stroke: Migraine with aura is associated with a slightly increased risk of ischemic stroke, particularly in women who smoke or use hormonal contraceptives.
Obesity: Chronic inflammation and metabolic dysfunction in obesity may worsen migraine frequency and severity.
Sleep Disorders (Insomnia, Sleep Apnea): Disrupted sleep patterns are a well-documented migraine trigger.
5. Medication Overuse and Rebound Headaches
Ironically, frequent use of pain relievers (e.g., NSAIDs, triptans, opioids, or caffeine-containing medications) can lead to medication-overuse headaches (MOH), worsening migraine frequency. This creates a vicious cycle where patients take more medication, only to experience rebound headaches when the drugs wear off.
Migraines are complex neurological events that often progress through distinct stages, each with its own set of symptoms. Not everyone experiences all stages, but understanding them can help in early recognition and management. The four main migraine stages are:
The prodrome stage, also known as the "premonitory phase," occurs hours or even days before the headache begins. During this stage, subtle warning signs may appear, signaling an impending migraine. Common symptoms include mood changes (such as irritability or depression), food cravings (especially for sweets), increased thirst, frequent yawning, neck stiffness, and heightened sensitivity to light or sound. Some people may also experience fatigue, difficulty concentrating, or digestive issues like constipation or diarrhea. Recognizing these early signs can allow for preventive measures, such as taking medication, staying hydrated, or avoiding known triggers.
Not all migraine sufferers experience aura, but for those who do, it typically occurs shortly before or during the headache phase. Aura symptoms are usually visual but can also involve other sensory or motor disturbances. Visual auras may include flashing lights, zigzag patterns, blind spots, or temporary vision loss. Sensory auras can cause tingling or numbness in the face, hands, or limbs, while language auras may lead to difficulty speaking or understanding words. These symptoms usually develop gradually over several minutes and can last up to an hour. Though aura can be alarming, it is generally harmless and resolves on its own as the migraine progresses.
The headache phase is often the most debilitating part of a migraine, lasting anywhere from a few hours to several days. The pain is typically throbbing or pulsating and usually affects one side of the head, though it can spread or switch sides. This stage is frequently accompanied by nausea, vomiting, extreme sensitivity to light (photophobia), sound (phonophobia), and sometimes smells. Physical activity often worsens the pain, leading many sufferers to seek rest in a dark, quiet room. The intensity can range from moderate to severe, making daily activities nearly impossible. Some people also experience dizziness, confusion, or even fainting during this phase. Proper pain management, hydration, and rest are crucial during this stage.
After the headache subsides, the postdrome phase—sometimes called the "migraine hangover"—sets in. This stage can last for hours or even a day or two. People often feel exhausted, weak, or mentally foggy, as if their brain is "wiped out." Some report lingering sensitivity to light and sound, while others may feel unusually refreshed or euphoric. Physical movement might still feel difficult, and concentration may remain impaired. Proper recovery involves rest, hydration, and gentle nutrition to help the body fully recuperate.
Diagnosing migraines involves a comprehensive evaluation of a patient's medical history, symptoms, and, in some cases, diagnostic tests to rule out other conditions. Since migraines do not have a specific laboratory test or imaging study for confirmation, healthcare providers rely on clinical criteria and patient-reported symptoms to make an accurate diagnosis.
1. Medical History and Symptom Assessment: The first step in diagnosing migraines is a detailed medical history, where the doctor asks about the frequency, duration, and characteristics of headaches. Key symptoms that support a migraine diagnosis include throbbing or pulsating pain, typically on one side of the head, along with nausea, vomiting, and sensitivity to light (photophobia) or sound (phonophobia). The presence of an aura—temporary visual, sensory, or speech disturbances before the headache—further supports the diagnosis. Doctors may also inquire about family history, as migraines often have a genetic component.
2. Diagnostic Criteria (ICHD-3 Guidelines): The International Classification of Headache Disorders (ICHD-3) provides standardized criteria for migraine diagnosis. According to these guidelines, a patient must have at least five headache attacks lasting 4–72 hours (untreated or unsuccessfully treated) with at least two of the following features: unilateral location, pulsating quality, moderate to severe intensity, or worsening with physical activity. Additionally, the headache must be accompanied by at least one of nausea/vomiting or sensitivity to light and sound. For migraines with aura, specific neurological symptoms must be present and reversible.
3. Physical and Neurological Examination: A thorough physical and neurological exam helps rule out other causes of headaches, such as infections, tumors, or vascular disorders. The doctor may check for abnormalities in vision, reflexes, coordination, and muscle strength. If red flags such as sudden severe headache, fever, seizures, or neurological deficits are present, further testing may be required to exclude serious conditions like stroke or meningitis.
4. Imaging and Additional Tests (If Needed): While migraines are typically diagnosed based on clinical assessment, imaging tests like MRI or CT scans may be ordered if the symptoms are atypical or if secondary causes are suspected. Blood tests or lumbar punctures (spinal taps) might also be performed to exclude infections, inflammation, or other underlying disorders. These tests are not routine but are used when the diagnosis is uncertain.
5. Differential Diagnosis: Migraines can mimic other headache disorders, such as tension-type headaches, cluster headaches, or sinus headaches. They must also be distinguished from secondary headaches caused by conditions like high blood pressure, brain tumors, or temporal arteritis. A careful evaluation ensures that the correct diagnosis is made and appropriate treatment is provided.
The International Classification of Headache Disorders (ICHD-3) criteria help confirm a migraine diagnosis.
While migraines are chronic, they can often be managed effectively with the right treatment. Some people experience fewer attacks as they age, while others may have persistent symptoms. Early intervention improves quality of life.
Migraines are more than just headaches—they are a debilitating neurological disorder affecting millions worldwide. Proper treatment involves a combination of acute relief strategies and long-term preventive measures. This article will explore in detail the various medications and approaches used to manage migraines, ensuring patients and medical students understand the options available.
When a migraine attack occurs, the primary goal is to stop the pain and associated symptoms as quickly as possible. The choice of medication depends on migraine severity, patient response, and any underlying health conditions.
For mild to moderate migraines, OTC medications can be effective:
NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): Ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin help reduce inflammation and pain.
Acetaminophen (Tylenol): Useful for patients who cannot tolerate NSAIDs, though it may be less effective for severe migraines.
Caffeine-Containing Combinations: Some OTC migraine formulas (Excedrin Migraine) combine aspirin, acetaminophen, and caffeine, which can enhance pain relief by improving drug absorption and constricting blood vessels.
However, overuse of OTC medications (more than 2-3 times per week) can lead to medication-overuse headaches, worsening the condition.
If OTC drugs are ineffective, stronger prescription options are available:
A. Triptans (Serotonin Receptor Agonists)
Triptans are the gold standard for acute migraine treatment, effective in about 70% of patients. They work by:
Constricting dilated blood vessels in the brain.
Blocking pain signals in the trigeminal nerve.
Reducing inflammation.
Common Triptans:
Sumatriptan (Imitrex): Available as oral tablets, nasal spray, or injectable form (fastest relief).
Rizatriptan (Maxalt): Dissolvable tablets for quicker absorption.
Eletriptan (Relpax), Zolmitriptan (Zomig), Almotriptan (Axert): Vary in onset and duration.
Side Effects:
Tingling, dizziness, chest tightness (not heart-related but should be used cautiously in cardiovascular patients).
Not recommended for those with uncontrolled hypertension or history of stroke.
B. Gepants (CGRP Receptor Antagonists)
For patients who cannot take triptans or do not respond to them, gepants offer an alternative:
Ubrogepant (Ubrelvy), Rimegepant (Nurtec): Block CGRP, a protein involved in migraine pain transmission.
Can be taken even late into a migraine attack.
No vasoconstrictive effects, making them safer for cardiovascular patients.
C. Ditans (Selective Serotonin 1F Receptor Agonists)
Lasmiditan (Reyvow): Unlike triptans, it does not constrict blood vessels, reducing cardiovascular risks.
May cause dizziness or sedation, so patients should avoid driving after taking it.
D. Anti-Nausea Medications
Since migraines often cause nausea/vomiting, these drugs help:
Metoclopramide (Reglan): Enhances stomach emptying, improving absorption of oral migraine drugs.
Prochlorperazine (Compazine), Promethazine (Phenergan): Reduce nausea and vomiting.
E. Ergots (Less Commonly Used Today)
Dihydroergotamine (DHE-45, Migranal): Effective but can cause severe side effects (nausea, vasospasm).
Usually reserved for patients unresponsive to other treatments.
If migraines are frequent (≥4 attacks/month), disabling, or poorly responsive to acute treatments, preventive therapy is recommended.
Beta-Blockers
Propranolol (Inderal), Metoprolol (Lopressor), Timolol: Reduce migraine frequency by stabilizing blood vessels and decreasing excitability in the brain.
Side effects: Fatigue, dizziness, low blood pressure.
Calcium Channel Blockers
Verapamil (Calan): Less effective than beta-blockers but an option for patients with asthma (since beta-blockers can worsen it).
Tricyclic Antidepressants (TCAs)
Amitriptyline, Nortriptyline: Help by increasing serotonin/norepinephrine levels, reducing pain sensitivity.
Side effects: Dry mouth, drowsiness, weight gain.
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
Venlafaxine (Effexor): Alternative for patients who cannot tolerate TCAs.
Topiramate (Topamax): Reduces neuronal hyperexcitability; effective but can cause cognitive side effects ("brain fog").
Valproate (Depakote): Used less due to risks of weight gain, tremors, and birth defects.
These are injectable drugs specifically designed for migraine prevention:
Erenumab (Aimovig), Fremanezumab (Ajovy), Galcanezumab (Emgality): Block CGRP activity, reducing migraine frequency.
Administered monthly or quarterly via self-injection.
Fewer side effects compared to traditional preventives.
Approved for chronic migraines (≥15 headache days/month).
Injected every 12 weeks into specific head/neck muscles.
Lifestyle Modifications: Regular sleep, hydration, avoiding triggers (certain foods, stress).
Biofeedback & Relaxation Techniques: Helps control physiological responses to stress.
Cognitive Behavioral Therapy (CBT): Addresses psychological triggers.
Preventing migraines involves a combination of lifestyle modifications, trigger avoidance, and pharmacological interventions. The goal is to reduce the frequency, severity, and duration of migraine attacks.
Many migraine sufferers find that certain lifestyle changes help in prevention:
Regular Sleep Patterns: Disrupted sleep or insufficient sleep can trigger migraines. Maintaining a consistent sleep schedule (7-9 hours per night) is essential.
Hydration and Diet: Dehydration is a common migraine trigger. Drinking enough water and avoiding caffeine, alcohol, aged cheeses, processed meats (containing nitrates), and artificial sweeteners (like aspartame) can help.
Stress Management: Stress is a major migraine trigger. Techniques such as yoga, meditation, deep breathing exercises, and cognitive behavioral therapy (CBT) can reduce stress-induced migraines.
Regular Exercise: Moderate aerobic exercise (e.g., walking, swimming) can help prevent migraines by improving blood flow and reducing stress. However, excessive or intense exercise may trigger attacks in some individuals.
Keeping a migraine diary helps identify personal triggers, which may include:
Hormonal changes (e.g., menstrual cycles, menopause)
Environmental factors (bright lights, loud noises, strong smells, weather changes)
Dietary triggers (chocolate, red wine, MSG)
Medications (oral contraceptives, vasodilators)
For patients with frequent or severe migraines (≥4 attacks per month), preventive medications may be prescribed. These include:
Beta-blockers (Propranolol, Metoprolol): Reduce blood vessel dilation and are effective in migraine prevention.
Antidepressants (Amitriptyline): Help regulate serotonin levels, which play a role in migraines.
Anticonvulsants (Topiramate, Valproate): Stabilize nerve activity in the brain.
CGRP Inhibitors (Erenumab, Fremanezumab): Newer monoclonal antibodies that block calcitonin gene-related peptide (CGRP), a key molecule in migraine pathways.
Botox (OnabotulinumtoxinA): Approved for chronic migraines (≥15 headache days per month), injected every 12 weeks to prevent attacks.
Some patients benefit from:
Magnesium, Riboflavin (Vitamin B2), and Coenzyme Q10 supplements (shown to reduce migraine frequency in studies).
Acupuncture: May help by stimulating nerve pathways involved in pain modulation.
Biofeedback: Teaches patients to control physiological responses (e.g., muscle tension) that may trigger migraines.
While migraines are often episodic, they can lead to serious complications if not properly managed. These complications can be categorized into acute, chronic, and long-term neurological effects.
This is a debilitating, prolonged migraine attack lasting more than 72 hours despite treatment. It often leads to:
Severe dehydration (due to persistent vomiting).
Hospitalization for IV fluids, corticosteroids, or stronger pain relief (e.g., IV dihydroergotamine or nerve blocks).
Also called rebound headache, this occurs when patients overuse acute migraine medications (e.g., triptans, NSAIDs, opioids) more than 10-15 days per month. Symptoms include:
Daily or near-daily headaches that worsen with medication withdrawal.
Treatment involves tapering off the overused drug and switching to preventive therapies.
When migraines occur ≥15 days per month for more than 3 months, they are classified as chronic migraines. This leads to:
Disability in work, social life, and mental health.
Increased risk of anxiety, depression, and sleep disorders.
Though rare, migraines—especially with aura—are associated with a higher risk of ischemic stroke. Mechanisms include:
Cortical Spreading Depression (CSD): A wave of neuronal depolarization that may trigger blood vessel constriction.
Hypercoagulability and endothelial dysfunction increasing clot formation.
Women under 45 with aura, smokers, and those on oral contraceptives are at higher risk.
A rare complication where aura symptoms (visual disturbances, tingling) last more than a week without stroke evidence on imaging. This may indicate prolonged neuronal hyperexcitability.
Chronic migraines are strongly linked to:
Depression and anxiety (due to chronic pain and disability).
Increased suicide risk in severe, untreated cases.
Studies suggest migraine sufferers (especially with aura) have a higher likelihood of:
Hypertension
Heart disease
Patent foramen ovale (PFO), a heart defect linked to stroke in migraine patients
Frequent migraines can lead to:
Gastroparesis (delayed stomach emptying) due to overuse of NSAIDs or vomiting.
Peptic ulcers from prolonged NSAID use.
Migraines are more than just headaches—they’re a complex neurological condition that requires proper understanding and management. By recognizing migraine symptoms and signs, identifying causes and risk factors, and following effective treatment and prevention strategies, sufferers can regain control over their lives.
If you experience frequent or severe migraines, consult a healthcare provider for a personalized treatment plan. With the right approach, migraines don’t have to dictate your life.
Migraines are complex neurological conditions influenced by various factors, including genetics, hormonal changes (especially in women), stress, certain foods (like aged cheese, processed meats, or MSG), dehydration, lack of sleep, bright lights, strong smells, and weather changes. Abnormal brain activity affecting nerve signals and blood vessels may also trigger migraines.
Preventing migraines involves identifying and avoiding triggers, maintaining a regular sleep schedule, staying hydrated, managing stress (through yoga or meditation), and eating balanced meals. Some people benefit from preventive medications (like beta-blockers or anticonvulsants) prescribed by a doctor.
A typical migraine lasts 4 to 72 hours if untreated. The duration varies: some experience short episodes, while others suffer for days. Migraines often progress through phases (prodrome, aura, attack, postdrome), prolonging discomfort.
There’s no instant cure, but treatments include:
Medications: Triptans (e.g., sumatriptan), NSAIDs (ibuprofen), or anti-nausea drugs.
Lifestyle changes: Cold compresses, dark/quiet rooms, caffeine in moderation, or acupuncture.
Preventive care: Regular exercise and avoiding triggers.
While most migraines aren’t life-threatening, chronic migraines can severely impact quality of life. Rarely, they may signal underlying conditions (e.g., strokes or aneurysms). Seek emergency care for sudden, severe headaches or neurological symptoms (e.g., slurred speech).
Chocolate is a common trigger for some due to caffeine and phenylethylamine. However, dark chocolate (in moderation) might help others by boosting serotonin. Monitor personal reactions.
Water: Dehydration is a major cause.
Ginger tea: Reduces inflammation and nausea.
Peppermint tea: Soothes tension headaches.
Electrolyte drinks: Replenish minerals lost during migraines.
Over-the-counter painkillers: Aspirin, ibuprofen, or acetaminophen.
Caffeine: Small amounts (e.g., coffee) can enhance painkiller effects.
Essential oils: Peppermint or lavender applied to temples.
Rest: Sleeping in a dark, quiet room.
Milk provides riboflavin (B2), which may prevent migraines in some. However, dairy can trigger headaches in lactose-intolerant individuals. Opt for almond or oat milk if sensitive.
Bananas: High in magnesium and potassium.
Watermelon: Hydrates and contains electrolytes.
Avocados: Rich in healthy fats and riboflavin.
Cherries: Anti-inflammatory properties.
For mild headaches: Acetaminophen (Tylenol) or ibuprofen (Advil).
For migraines: Triptans (e.g., Imitrex) or NSAIDs (naproxen).
Preventive options: Beta-blockers (propranolol) or Botox (for chronic cases).
Yes! Dehydration is a top trigger. Drinking water can alleviate or prevent attacks. Aim for 8–10 glasses daily, and add electrolytes if needed.