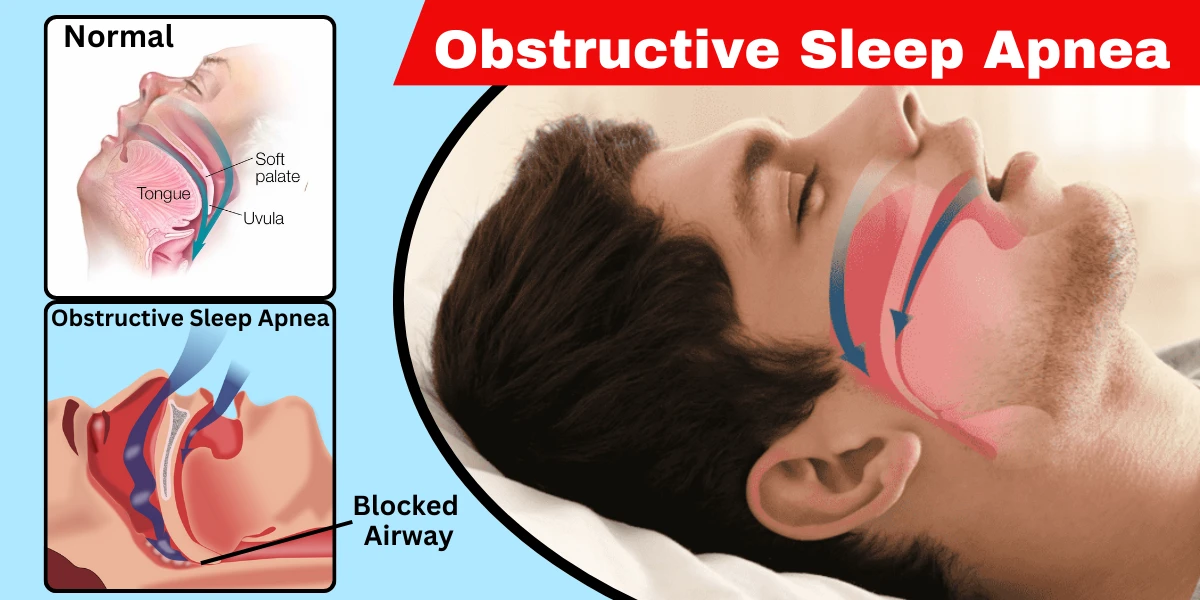
Obstructive sleep apnea (OSA) is a common but serious sleep disorder where breathing repeatedly stops and starts during sleep due to a blocked airway. Unlike central sleep apnea—where the brain fails to send proper signals to the muscles controlling breathing—OSA occurs when throat muscles relax excessively, obstructing airflow.
This condition affects millions worldwide, often going undiagnosed because symptoms like snoring or daytime fatigue are mistakenly dismissed as normal. Left untreated, OSA can lead to severe health complications, including heart disease, high blood pressure, and stroke.
Obstructive sleep apnea (OSA) is a widespread but often undiagnosed sleep disorder characterized by repeated interruptions in breathing during sleep. These pauses, called apneas, occur when the muscles in the throat relax excessively, causing a partial or complete blockage of the airway. When breathing stops, oxygen levels drop, triggering the brain to briefly wake the person to reopen the airway—often with a gasp or choking sound. These disruptions can happen dozens or even hundreds of times per night, severely impacting sleep quality and overall health.
Unlike central sleep apnea, where the brain fails to send proper signals to the muscles that control breathing, OSA is purely a mechanical issue. The airway collapses due to physical obstructions, such as excess throat tissue, a large tongue, or relaxed muscles. This leads to fragmented sleep, chronic fatigue, and long-term cardiovascular strain.
Obstructive sleep apnea (OSA) is classified into different types based on severity, which helps doctors determine the best treatment approach. The main categories are mild, moderate, and severe OSA, each defined by the number of breathing interruptions (apneas) per hour during sleep, measured by the Apnea-Hypopnea Index (AHI).
Mild OSA is diagnosed when a person experiences 5 to 14 breathing interruptions per hour. At this stage, symptoms may be subtle—occasional snoring, slight daytime fatigue, or brief awakenings that the person might not remember. Many people with mild OSA dismiss these signs as normal sleep disturbances or stress-related fatigue. However, even mild OSA can affect overall health, increasing the risk of high blood pressure and cardiovascular strain over time. Lifestyle changes, such as weight loss, positional therapy (sleeping on the side), and avoiding alcohol before bed, can often manage mild OSA effectively.
Moderate OSA is defined by 15 to 30 breathing interruptions per hour. At this stage, symptoms become more noticeable—louder snoring, frequent gasping for air at night, morning headaches, and significant daytime sleepiness. People with moderate OSA often struggle with concentration, memory lapses, and mood swings due to poor sleep quality. Since the airway obstruction is more severe, doctors may recommend Continuous Positive Airway Pressure (CPAP) therapy or oral appliances to keep the airway open during sleep. If left untreated, moderate OSA can progress to severe OSA and increase the risk of heart disease and stroke.
Severe OSA is the most critical form, with more than 30 breathing interruptions per hour. People with severe OSA experience frequent choking episodes, extreme fatigue, and a higher likelihood of falling asleep unintentionally during the day (even while driving or working). The repeated drops in oxygen levels put immense stress on the heart and brain, raising the risk of hypertension, heart failure, and stroke. Treatment for severe OSA almost always requires CPAP therapy, and in some cases, surgical interventions (such as UPPP, tonsillectomy, or Inspire implant) may be necessary if other treatments fail.
In addition to severity, OSA can also be categorized based on its underlying cause:
Understanding the type and severity of OSA is crucial for effective treatment. If you suspect you have sleep apnea, a sleep study (polysomnography) can provide a definitive diagnosis and guide the right treatment plan. Early intervention can prevent complications and significantly improve quality of life.
Obstructive sleep apnea (OSA) often goes undiagnosed because its symptoms occur during sleep, and many people dismiss them as normal fatigue or stress. However, recognizing these signs early can prevent serious health complications. Below, we break down the most common Obstructive Sleep Apnea Symptoms and Signs in detail.
One of the most noticeable signs of OSA is loud, persistent snoring, often disruptive enough to wake a sleeping partner. Unlike occasional snoring caused by a cold or allergies, OSA-related snoring is frequent and may include gasping or choking sounds as breathing restarts. The snoring happens because relaxed throat muscles partially block the airway, causing vibrations. However, not everyone who snores has sleep apnea—but if snoring is paired with other symptoms (like daytime fatigue), it’s worth investigating.
A classic symptom of OSA is suddenly waking up gasping for air, sometimes with a loud snort or choking sensation. This happens when the brain detects low oxygen levels and forces a brief awakening to reopen the airway. Many people don’t remember these episodes, but a bed partner may notice them. Frequent gasping at night is a strong indicator of sleep apnea and should not be ignored.
People with OSA often feel extremely tired during the day, even after a full night’s sleep. This happens because frequent breathing interruptions prevent deep, restorative sleep. Some may:
Fall asleep unintentionally (while working, watching TV, or even driving)
Struggle with poor concentration and memory lapses ("brain fog")
Feel constantly fatigued, no matter how much they sleep
This symptom is particularly dangerous because it increases the risk of car accidents and workplace errors.
While some OSA sufferers don’t recall waking up, others experience repeated nighttime awakenings, often with a racing heart or sense of panic. These disruptions prevent the body from reaching deep sleep stages, leading to non-refreshing sleep. Even if you don’t remember waking up, frequent trips to the bathroom at night (nocturia) can also be a hidden sign of OSA.
Waking up with a dull, throbbing headache is common in OSA due to low oxygen levels and increased carbon dioxide in the blood overnight. Additionally, many people with sleep apnea breathe through their mouths while sleeping, leading to:
Extreme dry mouth
Sore throat
Bad breath
These symptoms often improve once OSA is treated.
Chronic sleep deprivation from OSA can lead to:
Irritability and short temper
Anxiety or depression
Difficulty managing stress
Studies show that untreated sleep apnea doubles the risk of mood disorders because poor sleep disrupts brain chemicals like serotonin and dopamine.
OSA causes sudden drops in blood oxygen, forcing the heart to work harder. Over time, this leads to hypertension (high blood pressure), particularly in people whose blood pressure remains high despite medication. Research suggests that nearly 50% of people with hypertension also have undiagnosed sleep apnea.
Obstructive sleep apnea (OSA) occurs when the muscles in the throat relax too much during sleep, leading to a partial or complete blockage of the airway. This obstruction causes breathing to stop temporarily, often resulting in loud snoring, gasping, or sudden awakenings. While the immediate cause is physical airway blockage, several underlying risk factors contribute to the development and worsening of OSA.
One of the most significant risk factors for OSA is being overweight or obese. Fat deposits around the neck and upper airway can physically narrow the breathing passage, making it easier for the airway to collapse during sleep. Studies show that over 60% of people with OSA are overweight, and even a 10% weight loss can significantly reduce symptoms. Obesity also contributes to increased inflammation and reduced muscle tone in the throat, further worsening airway obstruction.
Some people are born with a naturally narrow throat or have structural abnormalities that increase OSA risk. Common anatomical causes include:
Enlarged tonsils or adenoids (common in children with OSA)
A deviated septum (crooked nasal passage that restricts airflow)
A recessed jaw (retrognathia) or large tongue that blocks the airway
A thicker neck circumference (men with a neck size >17 inches and women >16 inches are at higher risk)
These structural issues can make it harder for air to flow freely, even without excess weight.
OSA becomes more common with age because throat muscles naturally lose tone over time, making them more likely to collapse during sleep. Additionally:
Men are 2-3 times more likely to develop OSA than women, partly due to differences in fat distribution and airway structure.
Women’s risk increases after menopause, likely due to hormonal changes that affect muscle tone and weight distribution.
Certain habits and lifestyle choices can worsen or trigger OSA, including:
Alcohol and sedative use – These substances relax throat muscles excessively, increasing airway collapse.
Smoking – Irritates and inflames the upper airway, contributing to obstruction.
Poor sleep posture – Sleeping on the back (supine position) allows gravity to pull the tongue and soft tissues backward, blocking the airway.
Several health conditions are strongly associated with OSA, such as:
Hypertension (high blood pressure) – OSA causes repeated oxygen drops, straining the cardiovascular system.
Type 2 diabetes – Insulin resistance and obesity create a cycle that worsens OSA.
Hypothyroidism – Low thyroid function can lead to weight gain and muscle weakness in the throat.
Chronic nasal congestion (from allergies or sinus issues) – Forces mouth breathing, which increases airway instability.
OSA doesn’t have a single cause—it’s usually a combination of anatomical, lifestyle, and medical factors. While some risks (like genetics or age) can’t be changed, others (such as weight, alcohol use, and smoking) are modifiable. Understanding these Obstructive Sleep Apnea Causes and Risk Factors is the first step toward prevention and effective treatment.
If you have multiple risk factors, a sleep study can help determine whether you have OSA and how severe it is. Early intervention can prevent long-term complications like heart disease and cognitive decline.
Obstructive sleep apnea (OSA) doesn’t develop overnight—it progresses in stages, often worsening over time if left untreated. Understanding these stages helps in early detection and intervention, preventing severe complications. Below is a deeper look at how OSA evolves:
Stage 1: Occasional Snoring (Pre-OSA or Mild Snoring)
At this stage, the person may snore occasionally, especially when sleeping on their back or after alcohol consumption. The airway narrows slightly, but breathing interruptions are rare. Many dismiss this as normal, but it can be an early warning sign. Partners might notice inconsistent snoring, but the sleeper usually doesn’t wake up gasping. Lifestyle changes—such as weight management, avoiding alcohol before bed, and adjusting sleep position—can often prevent progression.
Stage 2: Chronic Snoring with Mild OSA (5-14 Apneas per Hour)
Here, snoring becomes more frequent and louder, accompanied by brief pauses in breathing (apneas) that last 10 seconds or longer. The brain briefly wakes the person to restart breathing, though they may not remember it. Daytime symptoms like mild fatigue or morning headaches may appear. A sleep study at this stage often confirms mild OSA. Treatment may include oral appliances, positional therapy, or a low-pressure CPAP machine if symptoms disrupt sleep quality.
Stage 3: Moderate OSA (15-30 Apneas per Hour)
Breathing interruptions become more frequent, leading to significant oxygen drops and sleep fragmentation. The person may wake up choking or gasping multiple times per night. Daytime sleepiness becomes harder to ignore, affecting concentration, mood, and productivity. High blood pressure and heart strain may develop due to repeated oxygen deprivation. A CPAP machine is often prescribed at this stage, and weight loss becomes critical if obesity is a contributing factor.
Stage 4: Severe OSA (30+ Apneas per Hour)
In severe cases, breathing stops more than 30 times per hour, sometimes for over a minute each time. Oxygen levels plummet, putting extreme stress on the heart and brain. The sleeper may experience severe morning headaches, memory problems, and a heightened risk of heart disease or stroke. Excessive daytime sleepiness can be dangerous, increasing the risk of car accidents. Treatment at this stage almost always requires a CPAP or BiPAP machine, and in some cases, surgery (like jaw advancement or Inspire therapy) may be considered.
Stage 5: End-Stage OSA (Life-Threatening Complications)
If still untreated, OSA can lead to life-threatening conditions like pulmonary hypertension, heart failure, or severe arrhythmias. Cognitive decline resembling dementia may occur due to chronic oxygen deprivation. At this point, aggressive treatment—including advanced PAP therapy, supplemental oxygen, or tracheostomy in extreme cases—is necessary to prevent fatal outcomes.
Why Recognizing the Stages Matters
The earlier OSA is diagnosed, the easier it is to manage. Mild cases may only require lifestyle adjustments, while severe OSA demands medical intervention. If you or someone you know exhibits worsening snoring, daytime fatigue, or unexplained health issues, a sleep study can determine the stage and guide treatment. Ignoring the progression can lead to irreversible damage, making timely action crucial.
Diagnosing obstructive sleep apnea (OSA) is crucial because many people remain unaware they have it. Since symptoms like snoring and daytime fatigue can be mistaken for normal tiredness, medical evaluation is necessary for confirmation. The diagnostic process typically involves a combination of clinical assessments, symptom analysis, and specialized sleep tests. Below, we explore the key methods used in Obstructive Sleep Apnea Diagnosis in greater detail.
Before ordering tests, doctors begin with a thorough medical history and physical exam. They will ask about:
Sleep habits (snoring, gasping, witnessed breathing pauses)
Daytime symptoms (fatigue, morning headaches, poor concentration)
Medical conditions (hypertension, diabetes, heart disease—all linked to OSA)
Lifestyle factors (alcohol use, smoking, weight changes)
A physical exam may check for:
Neck circumference (a thicker neck increases OSA risk)
Nasal obstruction (deviated septum, allergies)
Enlarged tonsils or uvula (common in some patients)
If OSA is suspected based on symptoms and risk factors, further testing is recommended.
The gold standard for diagnosing OSA is an overnight polysomnography (PSG) conducted in a sleep lab. During this test, sensors monitor:
Brain waves (EEG) – To track sleep stages
Breathing patterns – Detecting pauses (apneas) and shallow breaths (hypopneas)
Blood oxygen levels – Drops indicate interrupted breathing
Heart rate (ECG) – Irregularities may signal strain from OSA
Muscle activity (EMG) – Checks for limb movements disrupting sleep
Eye movements (EOG) – Helps identify REM sleep
A sleep specialist analyzes the data to determine:
Apnea-Hypopnea Index (AHI) – The number of breathing disruptions per hour (AHI ≥ 5 confirms OSA)
Severity level (Mild: 5–14, Moderate: 15–30, Severe: 30+)
While highly accurate, PSG can be expensive and inconvenient due to the overnight stay.
For patients with moderate to high OSA risk, a Home Sleep Apnea Test (HSAT) may be used. This portable device tracks:
Breathing effort (chest/abdomen movement)
Airflow (nasal cannula)
Blood oxygen levels (pulse oximeter)
Heart rate
Pros of HSAT:
More comfortable (done at home)
Lower cost than in-lab PSG
Useful for straightforward cases
Limitations:
Doesn’t record full sleep data (e.g., brain waves)
May underestimate AHI if sleep is fragmented
Not suitable for patients with other sleep disorders (e.g., insomnia, narcolepsy)
If results are inconclusive, an in-lab PSG may still be needed.
In some cases, doctors may recommend:
ENT Evaluation – An ear, nose, and throat (ENT) specialist checks for physical blockages (e.g., enlarged tonsils, nasal polyps).
Imaging (CT/MRI) – Rarely used but helpful if structural abnormalities (e.g., jaw misalignment) are suspected.
Daytime Sleepiness Tests – The Epworth Sleepiness Scale or Multiple Sleep Latency Test (MSLT) assesses excessive fatigue.
Why Early Diagnosis Matters
Undiagnosed OSA leads to:
Worsening cardiovascular risks (hypertension, stroke)
Cognitive decline (memory loss, poor focus)
Accidents (drowsy driving, workplace errors)
If you suspect OSA, consult a sleep specialist—timely diagnosis and treatment can drastically improve quality of life and long-term health.
The long-term outlook (prognosis) for obstructive sleep apnea (OSA) depends largely on early diagnosis and consistent treatment. When properly managed, most people with OSA experience significant improvements in sleep quality, daytime alertness, and overall health. Studies show that effective treatment—such as continuous positive airway pressure (CPAP) therapy—can reduce the risk of serious complications like heart disease, stroke, and diabetes.
However, untreated OSA tends to worsen over time. The repeated drops in oxygen levels and sleep disruptions strain the cardiovascular system, increasing the likelihood of hypertension, irregular heart rhythms, and even heart failure. Cognitive function may also decline due to chronic sleep deprivation, leading to memory problems and difficulty concentrating.
The good news? Patients who adhere to their prescribed treatment plan—whether CPAP, oral appliances, or lifestyle changes—often see a dramatic reduction in symptoms and associated health risks. Regular follow-ups with a sleep specialist are crucial to monitor progress and adjust treatment as needed.
Obstructive sleep apnea is a chronic condition, meaning it does not typically resolve on its own. Unlike temporary sleep disturbances (such as those caused by illness or stress), OSA persists unless actively treated. The duration of symptoms varies based on factors like:
Age & Muscle Tone – As people age, throat muscles naturally lose elasticity, which can worsen OSA if left untreated.
Weight Fluctuations – Gaining weight can exacerbate OSA, while losing it may improve (but not always cure) the condition.
Treatment Adherence – Those who consistently use CPAP or other therapies can effectively manage OSA indefinitely, preventing symptom progression.
While OSA is lifelong for most patients, its impact can be minimized with proper care. Some individuals—particularly those whose OSA is linked to reversible factors like obesity or nasal congestion—may see significant improvement or even resolution of symptoms with targeted interventions (e.g., weight loss, surgery, or allergy treatment). For others, long-term therapy is essential to maintain healthy breathing during sleep.
Obstructive sleep apnea (OSA) is a chronic condition, but the good news is that several effective treatments can significantly improve symptoms and reduce health risks. The right approach depends on the severity of OSA, underlying causes, and individual health factors. Below, we explore the most common Obstructive Sleep Apnea Treatment and Medication options in detail.
Lifestyle Modifications (First-Line Treatment for Mild OSA)
For individuals with mild OSA, lifestyle changes can often reduce or even eliminate symptoms. Weight loss is one of the most impactful strategies, as excess fat around the neck can compress the airway. Studies show that even a 10% reduction in body weight can dramatically improve breathing during sleep. Additionally, sleeping on your side (instead of your back) helps prevent the tongue and soft tissues from collapsing into the throat. Avoiding alcohol, sedatives, and heavy meals before bedtime is also crucial, as these relax throat muscles and worsen airway obstruction.
For those with nasal congestion due to allergies or a deviated septum, nasal strips, saline sprays, or antihistamines may help improve airflow. While lifestyle changes alone may not cure moderate to severe OSA, they can enhance the effectiveness of other treatments like CPAP therapy.
Continuous Positive Airway Pressure (CPAP) Therapy (Gold Standard for Moderate to Severe OSA)
CPAP machines are the most widely prescribed and effective treatment for moderate to severe OSA. A CPAP device delivers a steady stream of pressurized air through a mask, keeping the airway open during sleep. Many patients report immediate improvements in daytime alertness, reduced snoring, and better overall sleep quality after starting CPAP therapy.
However, some users struggle with mask discomfort or dryness. Modern CPAP machines now come with humidifiers and adjustable pressure settings to improve comfort. For those who find traditional CPAP challenging, BiPAP (Bilevel Positive Airway Pressure) machines offer variable pressure—higher when inhaling and lower when exhaling—making breathing feel more natural.
Despite its effectiveness, long-term CPAP compliance can be an issue, with about 30-50% of users discontinuing treatment due to discomfort. Working closely with a sleep specialist to find the right mask and settings can make a big difference.
Oral Appliances (Alternative for Mild to Moderate OSA or CPAP Intolerance)
For patients who cannot tolerate CPAP, mandibular advancement devices (MADs) are a popular alternative. These custom-fitted dental appliances reposition the lower jaw and tongue forward, preventing airway collapse. They are particularly helpful for people with mild to moderate OSA or those who travel frequently and find CPAP machines cumbersome.
While oral appliances are less effective than CPAP for severe OSA, studies show they reduce snoring and improve oxygen levels in many users. Potential side effects include jaw pain, tooth movement, or dry mouth, so regular follow-ups with a dentist specializing in sleep medicine are recommended.
Surgical Options (For Anatomical Obstructions or Treatment-Resistant Cases)
Surgery is typically considered when OSA is caused by physical blockages (like enlarged tonsils, a deviated septum, or excess throat tissue) and other treatments have failed. Common procedures include:
Uvulopalatopharyngoplasty (UPPP) – Removes excess tissue from the throat (tonsils, uvula, part of the soft palate).
Septoplasty/Turbinate Reduction – Corrects a deviated septum or swollen nasal turbinates to improve airflow.
Inspire Therapy – A surgically implanted device that stimulates the hypoglossal nerve to keep the airway open during sleep.
Maxillomandibular Advancement (MMA) – Repositions the jaw forward to enlarge the airway (often used in severe cases).
Success rates vary, and recovery can take weeks, so surgery is usually a last resort after CPAP and oral appliances have been tried.
Medications (Limited Role, Mostly for Symptom Management)
While no medication can cure OSA, some drugs help manage related symptoms:
Nasal Steroids or Decongestants – Reduce nasal congestion caused by allergies.
Modafinil/Armodafinil – Sometimes prescribed for excessive daytime sleepiness in patients still fatigued despite CPAP use.
Theophylline (Rarely Used) – A respiratory stimulant that may help in central sleep apnea but has limited effect on OSA.
Medications are not a standalone treatment but may be used alongside CPAP or other therapies.
Emerging and Experimental Treatments
Researchers are exploring new approaches, including:
Hypoglossal Nerve Stimulation – A pacemaker-like device that activates throat muscles during sleep (similar to Inspire but less invasive).
Myofunctional Therapy – Exercises to strengthen tongue and throat muscles, potentially reducing airway collapse.
Positional Therapy Devices – Wearable sensors that vibrate when you roll onto your back, encouraging side-sleeping.
While promising, these treatments require more research before becoming mainstream.
The best Obstructive Sleep Apnea Treatment and Medication plan depends on:
Severity of OSA (mild, moderate, or severe)
Anatomical factors (weight, neck size, nasal structure)
Lifestyle and preferences (ability to tolerate CPAP, willingness to try surgery)
A sleep specialist can help tailor a treatment strategy, whether it’s CPAP, an oral appliance, surgery, or a combination. The key is consistency—properly managing OSA can transform sleep quality, energy levels, and long-term health.
While some risk factors for obstructive sleep apnea (OSA), like genetics or age, can’t be changed, many lifestyle adjustments can significantly reduce your risk or even prevent mild cases from worsening. Here’s a deeper look at effective prevention strategies:
1. Maintain a Healthy Weight
Excess body weight, particularly around the neck, increases the likelihood of airway obstruction during sleep. Fat deposits in the throat can narrow the airway, making it easier for breathing to stop temporarily. Studies show that even a 10% reduction in body weight can dramatically improve or even eliminate OSA symptoms in overweight individuals. A balanced diet and regular exercise not only help with weight management but also improve overall muscle tone, including the muscles that keep the airway open.
2. Avoid Alcohol and Sedatives Before Bed
Alcohol, sleeping pills, and muscle relaxants cause the throat muscles to relax excessively, worsening airway collapse. If you’re at risk for OSA, it’s best to avoid alcohol at least 3-4 hours before bedtime. Similarly, consult your doctor about alternatives to sedatives if you rely on them for sleep.
3. Sleep Position Adjustments
Sleeping on your back (supine position) makes the tongue and soft tissues more likely to collapse backward, blocking airflow. Side sleeping is a simple yet effective way to reduce OSA risk. If you tend to roll onto your back, try using a special pillow or a tennis ball sewn into the back of your pajamas to discourage the habit. Some people also benefit from elevating the head of the bed slightly to improve airflow.
4. Treat Nasal Congestion Promptly
Chronic nasal congestion from allergies, sinus infections, or a deviated septum forces mouth breathing, which increases throat collapse risk. Saline sprays, antihistamines, or nasal steroid sprays can help keep nasal passages open. If structural issues (like a deviated septum) contribute to blockage, surgery may be an option.
5. Quit Smoking
Smoking irritates and inflames the upper airway, leading to swelling and fluid retention that narrow breathing passages. Research shows that smokers are three times more likely to develop OSA than non-smokers. Quitting smoking improves lung function and reduces inflammation, lowering OSA risk over time.
6. Strengthen Throat Muscles with Exercises
Weak throat muscles contribute to airway collapse. Simple oropharyngeal exercises, such as singing, playing wind instruments, or targeted tongue and throat exercises, can improve muscle tone. A 2015 study found that participants who performed daily throat exercises reduced snoring and mild OSA symptoms by nearly 40%.
7. Manage Underlying Medical Conditions
Certain health conditions, such as hypothyroidism, diabetes, and high blood pressure, are linked to higher OSA risk. Properly managing these conditions through medication, diet, and regular check-ups can help prevent sleep apnea from developing or worsening.
8. Establish a Consistent Sleep Routine
Poor sleep habits and irregular sleep schedules can worsen OSA by increasing throat muscle relaxation. Aim for 7-9 hours of quality sleep per night and maintain a consistent bedtime. A relaxing pre-sleep routine (such as reading or meditation) can also help reduce OSA-related disruptions.
9. Stay Hydrated
Dehydration can make throat tissues stickier and more prone to collapse. Drinking enough water throughout the day keeps mucous membranes moist, reducing airway resistance. However, avoid excessive fluids right before bed to minimize nighttime bathroom trips.
10. Regular Health Screenings
If you have risk factors (like a family history of OSA, obesity, or chronic snoring), consider a sleep study or consultation with a sleep specialist before symptoms become severe. Early detection allows for simpler interventions, such as lifestyle changes, before advanced treatments like CPAP are needed.
While not all cases of OSA can be prevented, these strategies significantly reduce risk and can even reverse mild sleep apnea. Combining weight management, smart sleep habits, and avoiding throat relaxants offers the best defense. If you suspect OSA despite preventive efforts, seek medical advice—early treatment prevents long-term complications.
Obstructive sleep apnea (OSA) doesn’t just disrupt sleep—it can lead to serious, sometimes life-threatening health complications if left untreated. The repeated pauses in breathing cause sudden drops in blood oxygen levels, putting immense strain on the cardiovascular system and other organs. Over time, this can contribute to chronic conditions that significantly reduce quality of life and longevity. Below, we explore the major complications associated with untreated OSA.
1. High Blood Pressure (Hypertension)
When breathing stops during sleep, oxygen levels drop, triggering the brain to briefly wake you up to restart breathing. This sudden stress response causes blood pressure to spike repeatedly throughout the night. Over time, these frequent surges can lead to chronic hypertension, increasing the risk of heart disease and stroke. Studies show that nearly 50% of people with OSA have high blood pressure, and those with severe OSA are three times more likely to develop resistant hypertension (hard-to-control high blood pressure).
2. Heart Disease and Stroke
The constant strain on the cardiovascular system from OSA can lead to more severe heart conditions. The lack of oxygen forces the heart to work harder, contributing to:
Coronary artery disease (narrowed or blocked heart arteries)
Heart attacks (due to reduced oxygen supply)
Atrial fibrillation (irregular heartbeat, increasing stroke risk)
Heart failure (weakened heart muscle from chronic stress)
Research indicates that people with untreated OSA are two to four times more likely to experience a stroke. The risk is even higher in those with severe OSA, as poor oxygen flow can damage blood vessels in the brain.
3. Type 2 Diabetes and Metabolic Syndrome
OSA is strongly linked to insulin resistance, a key factor in type 2 diabetes. Sleep deprivation and oxygen deprivation disrupt glucose metabolism, making it harder for the body to regulate blood sugar. Studies show that up to 80% of people with type 2 diabetes also have OSA, and treating sleep apnea can improve blood sugar control. Additionally, OSA contributes to metabolic syndrome—a cluster of conditions including high blood pressure, high blood sugar, excess body fat, and abnormal cholesterol levels.
4. Memory and Cognitive Decline
Chronic sleep fragmentation from OSA prevents the brain from entering deep, restorative sleep stages essential for memory consolidation and cognitive function. Over time, this can lead to:
Memory loss (similar to early dementia symptoms)
Poor concentration and brain fog
Increased risk of Alzheimer’s disease (studies show OSA accelerates brain aging)
A 2020 study found that people with untreated severe OSA had significantly higher levels of tau protein, a biomarker linked to Alzheimer’s.
5. Mood Disorders and Mental Health Issues
The constant sleep deprivation caused by OSA can severely impact mental health. Many patients experience:
Depression (due to chronic fatigue and poor sleep quality)
Anxiety (often from frequent nighttime awakenings)
Irritability and mood swings
Research suggests that nearly 1 in 3 people with OSA also suffer from depression, and treating sleep apnea can improve mood and emotional stability.
6. Increased Risk of Accidents
Daytime sleepiness from OSA significantly raises the risk of:
Car accidents (people with OSA are 2.5 times more likely to be in a crash)
Workplace injuries (especially in jobs requiring alertness, like driving or operating machinery)
Many countries now require commercial truck drivers with OSA to undergo treatment before being allowed to drive.
7. Liver Problems
OSA is linked to non-alcoholic fatty liver disease (NAFLD) and liver fibrosis. The intermittent hypoxia (low oxygen levels) triggers inflammation and oxidative stress, damaging liver cells over time.
Obstructive sleep apnea is far more than just loud snoring—it’s a serious medical condition with far-reaching consequences. From heart disease and stroke to diabetes, cognitive decline, and mental health struggles, untreated OSA can silently damage multiple systems in the body.
The good news? OSA is treatable. Whether through CPAP therapy, lifestyle changes, oral appliances, or surgery, effective treatments can drastically reduce symptoms and prevent complications. If you or a loved one experiences chronic snoring, daytime fatigue, or frequent nighttime awakenings, don’t ignore the signs—seek a sleep study and professional diagnosis.
Sleep apnea can be managed through lifestyle changes, medical devices, or surgery, depending on severity. Common treatments include:
CPAP (Continuous Positive Airway Pressure) machines.
Weight loss, if overweight.
Positional therapy (avoiding sleeping on your back).
Oral appliances to keep the airway open.
Surgery, in cases where anatomy obstructs breathing.
There’s no one-size-fits-all cure, so treatment must be tailored to the individual.
Yes, many people with sleep apnea live long lives—especially when the condition is diagnosed and treated properly. Untreated sleep apnea, however, significantly increases the risk of heart disease, stroke, diabetes, and high blood pressure, which can shorten lifespan.
Key warning signs include:
Loud, chronic snoring.
Gasping or choking during sleep.
Excessive daytime sleepiness.
Morning headaches.
Difficulty concentrating or memory problems.
Mood changes or irritability.
Waking up frequently at night to urinate.
The most common form, obstructive sleep apnea (OSA), is usually caused by airway obstruction due to relaxed throat muscles during sleep. Risk factors include:
Excess weight
Large neck circumference
Narrow airway
Smoking
Alcohol or sedative use
Family history
Yes. Sleep apnea is a serious medical condition that can lead to life-threatening complications if left untreated, including:
Heart attack
Stroke
Type 2 diabetes
Hypertension
Arrhythmias
Accidents due to daytime sleepiness
Yes, it’s often called a “silent killer” because symptoms like snoring and fatigue are frequently ignored, yet the condition increases the risk of sudden cardiac death, stroke, and other deadly complications.
Groups most affected include:
Men over 40
People who are overweight or obese
Postmenopausal women
Individuals with a family history
People with large tonsils or nasal obstruction
It can affect children and thin individuals too, but it’s more prevalent in the groups above.
Sleep apnea is typically a chronic condition, but in some cases it can be cured or significantly improved:
Weight loss may eliminate symptoms.
Surgical interventions can be curative for some anatomical issues.
Pediatric cases caused by enlarged tonsils may resolve after tonsillectomy.
However, most adults require ongoing management.
Dangers include:
Cardiovascular disease
High blood pressure
Diabetes
Depression and anxiety
Daytime fatigue, increasing accident risk
Cognitive decline and memory problems
Yes. Sleep apnea can cause brain damage over time due to repeated oxygen deprivation. It’s linked to:
Impaired memory and learning
Increased risk of dementia
Changes in brain structure and function, especially in untreated cases
The best sleeping position is on your side, particularly the left side. Sleeping on your back (supine) worsens apnea by allowing the tongue and soft tissues to block the airway. Some people benefit from:
Positional therapy
Wedge pillows
Specialized sleep apnea pillows
Sleep apnea can start at any age, including childhood. However, it is most common in adults aged 40 and older. In children, causes often include enlarged tonsils or adenoids. In adults, it's more related to lifestyle, weight, and age-related changes in muscle tone.