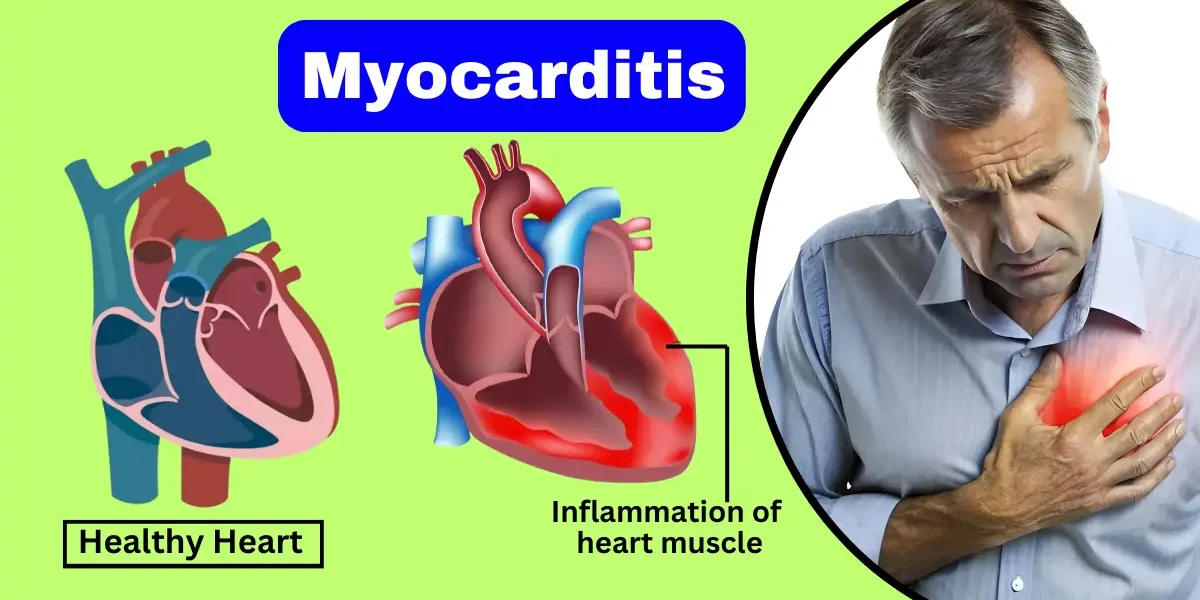
Myocarditis is a serious but often misunderstood heart condition that can affect people of all ages. It occurs when the heart muscle (myocardium) becomes inflamed, weakening its ability to pump blood efficiently. While some cases are mild and resolve on their own, others can lead to severe complications, including heart failure or sudden cardiac arrest.
Myocarditis is an inflammatory condition of the heart muscle (myocardium) that can weaken the heart's ability to pump blood efficiently. This inflammation can be caused by infections (most commonly viral), autoimmune diseases, toxic substances, or adverse reactions to medications. When the myocardium becomes inflamed, the heart may swell, leading to symptoms such as chest pain, fatigue, shortness of breath, and, in severe cases, heart failure or arrhythmias. Myocarditis can range from mild cases that resolve on their own to life-threatening conditions requiring immediate medical intervention. Early diagnosis and treatment are crucial to prevent long-term damage to the heart.
Myocarditis can be classified into different types based on its cause, duration, and severity:
Infectious Myocarditis – This is the most common type and is typically caused by viral infections, such as Coxsackievirus, Adenovirus, Parvovirus B19, or SARS-CoV-2 (COVID-19). Bacterial, fungal, and parasitic infections can also lead to myocarditis, though less frequently. The infection triggers an immune response that causes inflammation in the heart muscle.
Autoimmune Myocarditis – In some cases, the body's immune system mistakenly attacks the heart tissue, leading to chronic inflammation. This type is often associated with autoimmune diseases like lupus, rheumatoid arthritis, or giant cell myocarditis, a rare but aggressive form of the disease.
Toxic Myocarditis – Exposure to certain toxins, such as heavy metals, chemotherapy drugs (e.g., doxorubicin), or excessive alcohol consumption, can damage the heart muscle and cause inflammation. This type may develop gradually or suddenly, depending on the level of exposure.
Giant Cell Myocarditis – A rare and severe form of myocarditis characterized by the presence of giant cells (large, fused immune cells) in the heart tissue. It progresses rapidly and often leads to severe heart failure or life-threatening arrhythmias, requiring aggressive treatment such as immunosuppressive therapy or a heart transplant.
Eosinophilic Myocarditis – This type occurs when an excess of eosinophils (a type of white blood cell) infiltrates the heart muscle, often due to allergic reactions, parasitic infections, or certain medications. It can lead to tissue damage and impaired heart function.
Each type of myocarditis requires a specific diagnostic and treatment approach, depending on its underlying cause and severity. Early recognition and management are essential to prevent complications such as dilated cardiomyopathy or sudden cardiac arrest.
Myocarditis can be tricky to diagnose because its symptoms often mimic other common conditions, such as the flu or even a heart attack. The severity of symptoms varies widely—some people may feel only mild discomfort, while others experience life-threatening complications. Below, we break down the most common signs and symptoms of myocarditis in detail.
Chest Pain: One of the most alarming symptoms is chest pain, which can range from a dull ache to a sharp, stabbing sensation. Some patients describe it as a heavy pressure, similar to a heart attack. This pain occurs because the inflamed heart muscle isn’t getting enough oxygen, or because the surrounding tissue is irritated. Unlike typical heart attack pain, myocarditis-related discomfort may worsen when lying down or taking deep breaths.
Fatigue and Weakness: Since the heart struggles to pump efficiently during myocarditis, the body receives less oxygen-rich blood. This leads to extreme fatigue, even after minimal activity. Patients often report feeling unusually tired, weak, or dizzy—sometimes to the point where climbing stairs or walking short distances becomes exhausting.
Shortness of Breath: As the heart weakens, fluid can back up into the lungs, causing breathlessness. This symptom may start subtly—perhaps only during exercise—but can progress to difficulty breathing even at rest. In severe cases, patients may wake up gasping for air (a condition called paroxysmal nocturnal dyspnea) or need to sleep propped up on pillows to breathe comfortably.
Heart Palpitations and Irregular Heartbeat: Inflammation disrupts the heart’s electrical system, leading to arrhythmias (abnormal heart rhythms). Patients may feel their heart skipping beats, fluttering, or racing without explanation. Some arrhythmias are harmless, but others—like ventricular tachycardia—can be life-threatening and require immediate treatment.
Swelling (Edema) in the Legs, Ankles, or Feet: When the heart can’t pump effectively, fluid accumulates in the body’s tissues—a condition called edema. Swelling usually begins in the feet and ankles but can spread upward if heart function continues to decline. Pressing on the swollen area may leave a temporary indentation (a sign of pitting edema).
Flu-Like Symptoms: Because myocarditis often follows a viral infection, many patients first experience fever, muscle aches, sore throat, or headaches—symptoms easily mistaken for the flu. However, if these persist alongside heart-related issues (like chest pain or fatigue), myocarditis should be considered.
In extreme cases, myocarditis can lead to:
Fainting (syncope) due to irregular heart rhythms or low blood pressure.
Blue-tinged lips or fingers (cyanosis), signaling poor oxygen circulation.
Sudden collapse (in rare cases of severe arrhythmia or cardiac arrest).
If you or someone you know experiences:
✔ Severe, unexplained chest pain
✔ Difficulty breathing (especially at rest)
✔ Fainting or near-fainting episodes
✔ Rapid or irregular heartbeat that doesn’t resolve
...seek medical help immediately. Early intervention can prevent permanent heart damage.
Myocarditis affects people differently based on:
The cause (viral cases may start with flu-like symptoms, while autoimmune myocarditis might develop more slowly).
The extent of inflammation (mild vs. widespread damage).
Individual health (young, otherwise healthy people may recover faster, while those with preexisting conditions may face complications).
Myocarditis occurs when the heart muscle becomes inflamed, but what exactly triggers this condition? The causes can vary widely, from infections to autoimmune reactions, and understanding them is key to prevention and treatment. Below, we explore the primary causes of myocarditis and the risk factors that make certain individuals more susceptible.
1. Viral Infections (The Most Common Culprit)
The leading cause of myocarditis is viral infections. Viruses like coxsackievirus, adenovirus, parvovirus B19, and even COVID-19 can invade heart tissue, triggering inflammation. When your immune system fights off the infection, it sometimes mistakenly attacks healthy heart cells, worsening the damage. Studies suggest that up to 50% of myocarditis cases are linked to viral infections, making this the biggest risk factor.
2. Bacterial and Parasitic Infections (Less Common but Serious)
While viruses dominate the list, bacteria like Staphylococcus, Streptococcus, and Lyme disease-causing Borrelia burgdorferi can also lead to myocarditis. In tropical regions, parasites such as Trypanosoma cruzi (Chagas disease) are a notable cause. These infections are rarer but often more aggressive, requiring prompt treatment to prevent severe heart damage.
3. Autoimmune Diseases (When the Body Attacks Itself)
Conditions like lupus, rheumatoid arthritis, and giant cell myocarditis can cause the immune system to target the heart muscle. This form of myocarditis is particularly tricky because it’s not triggered by an external infection but by the body’s own defenses going haywire. Treatment often involves immunosuppressants to calm the overactive immune response.
4. Toxic Exposure (Drugs, Chemicals, and Heavy Metals)
Certain medications, including chemotherapy drugs (like doxorubicin), antibiotics, and even some antipsychotics, have been linked to myocarditis. Illicit drug use (especially cocaine and methamphetamine) and exposure to heavy metals like lead or mercury can also inflame the heart muscle. Even common over-the-counter drugs, like NSAIDs (ibuprofen, naproxen), have been associated with rare cases.
5. Allergic Reactions and Vaccines (Rare but Possible)
Severe allergic reactions (anaphylaxis) can sometimes lead to myocarditis due to a sudden immune system overload. Additionally, vaccine-related myocarditis, though extremely rare, has been reported—mostly in young males after mRNA COVID-19 vaccines. However, experts emphasize that the benefits of vaccination far outweigh this minimal risk.
While myocarditis can affect anyone, some groups are at higher risk:
Young Adults and Athletes – Intense physical exertion, especially after a viral illness, may increase the risk of myocarditis. This is why doctors often recommend resting after infections like the flu or COVID-19 before returning to strenuous exercise.
People with Weakened Immune Systems – Those with HIV/AIDS, diabetes, or undergoing chemotherapy are more susceptible because their bodies struggle to fight off infections that could trigger myocarditis.
Individuals with Autoimmune Diseases – Since their immune systems are already prone to attacking healthy tissue, they have a higher chance of developing myocarditis.
Recent Viral or Bacterial Illness – A recent bout of the flu, COVID-19, or another infection can precede myocarditis, making recovery periods crucial.
Why Understanding Causes and Risk Factors Matters
Recognizing the causes and risk factors of myocarditis helps in early detection and prevention. If you fall into a high-risk category—such as having an autoimmune disease or recently recovering from a viral infection—being aware of the symptoms and seeking prompt medical care can make a significant difference in outcomes.
Myocarditis progresses through distinct stages, each affecting the heart in different ways. Understanding these phases helps doctors determine the best treatment approach and predict potential outcomes. Below, we explore the three key stages of myocarditis in detail.
The acute stage occurs shortly after the initial injury or infection, typically caused by viruses (e.g., Coxsackievirus, adenovirus, SARS-CoV-2), bacteria, or autoimmune reactions. During this phase, the heart muscle becomes inflamed, leading to edema (swelling) and infiltration of immune cells (lymphocytes, macrophages). Symptoms may include chest pain, fatigue, palpitations, and shortness of breath. Some patients may experience mild symptoms, while others develop severe cardiac dysfunction. Diagnostic tests such as cardiac MRI, echocardiography, and troponin levels help identify inflammation and myocardial injury. Early treatment with anti-inflammatory medications or antivirals (if applicable) may help reduce damage.
In the subacute stage, the initial inflammation begins to subside, but the heart muscle may still show signs of injury. Fibrosis (scar tissue formation) starts to develop as the body attempts to repair damaged tissue. Some patients recover fully, while others progress to chronic myocarditis or dilated cardiomyopathy due to persistent inflammation. Symptoms may improve, but in some cases, arrhythmias or heart failure symptoms (e.g., fatigue, fluid retention) persist. Continued monitoring through imaging and biomarkers is essential to assess recovery or progression.
If inflammation persists or recurs, the condition enters the chronic stage, leading to progressive myocardial damage. Extensive fibrosis replaces healthy heart tissue, impairing the heart’s ability to pump blood efficiently. This stage often results in dilated cardiomyopathy (DCM), characterized by an enlarged, weakened heart. Patients may experience worsening heart failure, arrhythmias, or sudden cardiac death. Treatment focuses on managing heart failure (e.g., beta-blockers, ACE inhibitors) and preventing complications. In severe cases, advanced therapies like implantable devices (ICDs) or heart transplantation may be necessary.
Fulminant myocarditis is a life-threatening form that develops rapidly, often within hours to days. It causes severe inflammation, leading to cardiogenic shock, arrhythmias, and acute heart failure. Patients require immediate intensive care, including mechanical circulatory support (e.g., ECMO) or temporary ventricular assist devices. Despite its severity, those who survive the acute phase often recover better than those with chronic myocarditis, as the inflammation is intense but short-lived.
Diagnosing myocarditis can be challenging because its symptoms often overlap with other heart and respiratory conditions, such as a heart attack, pericarditis, or even a severe viral infection. Since early detection is crucial to preventing complications, doctors use a combination of medical history, physical exams, and advanced tests to confirm the diagnosis. Below, we explore the key diagnostic methods in detail.
1. Blood Tests
Blood tests are often the first step in evaluating myocarditis. Doctors look for specific markers that indicate heart muscle damage or inflammation. Elevated levels of troponin (a protein released when the heart is injured) and C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) (which signal inflammation) can suggest myocarditis. Additionally, tests for viral or bacterial infections (such as COVID-19, Lyme disease, or streptococcus) help identify potential causes.
2. Electrocardiogram (ECG or EKG)
An ECG measures the heart’s electrical activity and can detect irregularities that may point to myocarditis. Common findings include:
ST-segment or T-wave abnormalities (similar to those seen in a heart attack)
Arrhythmias (irregular heartbeats, such as atrial fibrillation or ventricular tachycardia)
Heart block (delayed electrical signals between the heart’s chambers)
While an ECG alone cannot confirm myocarditis, it provides important clues that guide further testing.
3. Echocardiogram (Cardiac Ultrasound)
An echocardiogram uses sound waves to create real-time images of the heart’s structure and function. Doctors look for:
Reduced ejection fraction (a sign that the heart isn’t pumping efficiently)
Wall motion abnormalities (areas of the heart muscle that aren’t contracting properly)
Fluid buildup around the heart (pericardial effusion, which can occur alongside myocarditis)
This test helps assess the severity of heart damage and rule out other conditions, such as valve disease or congenital defects.
4. Cardiac MRI (Magnetic Resonance Imaging)
A cardiac MRI is one of the most accurate tools for diagnosing myocarditis. It provides detailed images of the heart’s structure, inflammation, and scar tissue. Key features doctors look for include:
Edema (swelling) in the heart muscle
Late gadolinium enhancement (LGE) – A pattern that indicates inflammation or fibrosis (scarring)
Regional heart wall motion abnormalities
Because of its precision, cardiac MRI is often considered the gold standard for myocarditis diagnosis, especially in unclear cases.
5. Endomyocardial Biopsy (Invasive Testing)
In severe or uncertain cases, a doctor may recommend an endomyocardial biopsy, where a small tissue sample is taken from the heart muscle and examined under a microscope. This test can:
Confirm active inflammation (lymphocytic, eosinophilic, or giant cell myocarditis)
Identify infectious agents (such as viral DNA in the heart tissue)
Rule out other diseases (like amyloidosis or sarcoidosis)
However, biopsies are not always necessary because they are invasive and carry risks (e.g., bleeding, arrhythmias). They are typically reserved for high-risk patients or those not responding to treatment.
6. Additional Tests (When Needed)
Depending on the suspected cause, doctors may order:
Chest X-ray – To check for fluid in the lungs (a sign of heart failure)
Viral PCR or antibody testing – To detect specific infections (e.g., parvovirus, adenovirus)
Coronary angiography – To rule out blocked arteries (if symptoms mimic a heart attack)
Since myocarditis can range from mild to life-threatening, prompt diagnosis is critical. Misdiagnosis or delayed treatment can lead to chronic heart failure, dangerous arrhythmias, or even sudden cardiac arrest. If you experience unexplained chest pain, fatigue, or irregular heartbeats—especially after a recent infection—seek medical evaluation immediately.
The prognosis of myocarditis varies widely depending on several factors, including the underlying cause, the severity of inflammation, and how quickly treatment begins. While many people recover fully without long-term complications, others may face chronic heart issues or life-threatening conditions. Here’s a detailed look at what influences outcomes and what patients can expect.
The prognosis largely depends on:
The cause of myocarditis – Viral cases often resolve with supportive care, whereas autoimmune or giant cell myocarditis may require aggressive treatment.
The extent of heart damage – Mild inflammation may heal completely, but severe cases can lead to permanent scarring (fibrosis), weakening the heart muscle.
Timely diagnosis and treatment – Early intervention improves the chances of full recovery, while delays can result in progressive heart failure.
Patient health before myocarditis – Individuals with pre-existing heart conditions, weakened immune systems, or other chronic illnesses may have a more complicated recovery.
Full Recovery – Many patients, especially those with mild viral myocarditis, regain normal heart function within weeks to months. Athletes and young adults often recover well if they follow medical advice, including temporary rest from intense exercise.
Chronic Heart Issues – In some cases, persistent inflammation leads to dilated cardiomyopathy (an enlarged, weakened heart) or arrhythmias, requiring lifelong medication and monitoring.
Severe Complications – A small percentage of patients develop acute heart failure, cardiogenic shock, or life-threatening arrhythmias, which may necessitate advanced treatments like implantable defibrillators or even heart transplantation.
Even after recovery, patients should undergo regular follow-ups, including:
Echocardiograms to assess heart function.
Holter monitors to detect irregular heartbeats.
Blood tests to check for ongoing inflammation or heart strain.
Doctors may recommend avoiding strenuous exercise for several months to prevent relapse.
Studies show that:
About 50-80% of mild viral myocarditis cases resolve completely with proper care.
Up to 20% of patients develop chronic heart dysfunction.
Giant cell myocarditis has a poorer prognosis, with many patients requiring a heart transplant within five years.
The treatment for myocarditis depends on the underlying cause, severity of symptoms, and whether complications like heart failure or arrhythmias are present. Since myocarditis involves inflammation of the heart muscle, the primary goals of treatment are to:
Reduce inflammation
Support heart function
Treat the underlying cause (if identifiable)
Prevent complications
Here’s a detailed breakdown of the treatment approaches:
Doctors may prescribe different medications based on the type and stage of myocarditis:
Anti-inflammatory Drugs
Corticosteroids (e.g., prednisone): Used in severe or autoimmune-related myocarditis to suppress the immune system and reduce inflammation.
Nonsteroidal anti-inflammatory drugs (NSAIDs): Sometimes used in mild cases, but caution is needed as they may worsen some forms of myocarditis (e.g., viral).
Heart Failure Medications
ACE inhibitors or ARBs (e.g., lisinopril, losartan): Help relax blood vessels and reduce strain on the heart.
Beta-blockers (e.g., metoprolol, carvedilol): Slow the heart rate and decrease workload.
Diuretics (e.g., furosemide): Remove excess fluid to reduce swelling and ease breathing.
Antiviral or Antibiotic Therapy
If a viral or bacterial infection is the cause, doctors may prescribe antivirals (e.g., for COVID-19 or influenza) or antibiotics (e.g., for Lyme disease).
Immunosuppressants (for Autoimmune Myocarditis)
Drugs like azathioprine or IVIG (intravenous immunoglobulin) may be used if the immune system is attacking the heart.
Medications for Arrhythmias
If irregular heartbeats occur, antiarrhythmic drugs (e.g., amiodarone) or even a temporary pacemaker may be needed.
Rest and Activity Restrictions
Physical exertion can worsen myocarditis, so doctors often recommend avoiding intense exercise for 3-6 months (or longer for athletes).
Gradual return to activity is allowed only after heart function improves.
Low-Sodium Diet & Fluid Management
Reducing salt helps prevent fluid retention, easing strain on the heart.
Fluid intake may be restricted in severe cases to prevent overload.
Monitoring for Complications
Regular follow-ups with a cardiologist are crucial to check for heart failure or arrhythmias.
If myocarditis leads to life-threatening complications, more aggressive treatments may be required:
Mechanical Circulatory Support
Ventricular Assist Devices (VADs): Temporary pumps that help the heart circulate blood in severe heart failure.
Extracorporeal Membrane Oxygenation (ECMO): A machine that oxygenates blood outside the body when the heart is too weak to function.
Heart Transplant
In rare cases where the heart is irreversibly damaged, a transplant may be the only option.
Most people with mild myocarditis recover fully with proper treatment. However, some may develop chronic heart issues, requiring lifelong medication and monitoring. Key steps for recovery include:
Strict adherence to prescribed medications
Regular cardiac check-ups (echocardiograms, MRIs)
Gradual reintroduction of exercise under medical supervision
Preventing myocarditis primarily involves minimizing exposure to infectious agents, adopting a heart-healthy lifestyle, and ensuring timely medical intervention when necessary.
Many cases of myocarditis are caused by viral infections, including enteroviruses (e.g., Coxsackievirus), influenza, adenovirus, SARS-CoV-2 (COVID-19), and others. Vaccination plays a critical role in preventing these infections:
Influenza Vaccine: Annual flu shots reduce the risk of viral myocarditis triggered by influenza.
COVID-19 Vaccine: While rare cases of myocarditis have been reported post-mRNA vaccination (mostly in young males), the risk of myocarditis from COVID-19 infection itself is significantly higher. Thus, vaccination remains strongly recommended.
MMR (Measles, Mumps, Rubella) Vaccine: Prevents infections that could indirectly lead to myocarditis.
Polio and Hepatitis B Vaccines: These also reduce the risk of viral infections that may affect the heart.
Since many cases of myocarditis are viral, practicing good hygiene reduces transmission:
Frequent handwashing with soap and water.
Avoiding close contact with individuals who have respiratory or gastrointestinal infections.
Proper food handling to prevent enterovirus infections.
If a bacterial infection (e.g., Lyme disease, streptococcal infections) is suspected, early antibiotic treatment can prevent secondary myocarditis. Similarly, antiviral medications may be considered in certain high-risk viral infections.
Alcohol and Drugs: Excessive alcohol can lead to toxic myocarditis. Illicit drugs (e.g., cocaine, amphetamines) can cause direct heart muscle damage.
Certain Medications: Some chemotherapy drugs (e.g., doxorubicin) and immune checkpoint inhibitors can induce myocarditis. Close cardiac monitoring is essential in such cases.
Conditions like lupus, sarcoidosis, or giant cell myocarditis can trigger immune-mediated myocarditis. Proper treatment with immunosuppressants (e.g., corticosteroids, IVIG) may be necessary.
Patients with a history of myocarditis or those at high risk (e.g., athletes, immunocompromised individuals) should undergo periodic cardiac evaluations, including ECG, echocardiogram, or cardiac MRI, to detect early signs of heart dysfunction.
If myocarditis is not diagnosed early or managed properly, it can lead to severe and sometimes life-threatening complications:
1. Dilated Cardiomyopathy (DCM) and Heart Failure
Chronic inflammation weakens the heart muscle, leading to dilated cardiomyopathy, where the heart becomes enlarged and pumps inefficiently. Symptoms include:
Fatigue, shortness of breath (even at rest)
Swelling in legs (edema)
Fluid accumulation in lungs (pulmonary edema)
Treatment involves ACE inhibitors, beta-blockers, diuretics, and in severe cases, mechanical support (LVAD) or heart transplant.
2. Arrhythmias (Abnormal Heart Rhythms)
Inflammation disrupts the heart’s electrical system, leading to:
Atrial fibrillation (AFib) → Increased stroke risk
Ventricular tachycardia (VT) or fibrillation (VF) → Can cause sudden cardiac arrest
Heart block → May require a pacemaker
Management includes antiarrhythmic drugs, implantable cardioverter-defibrillator (ICD), or ablation therapy.
3. Sudden Cardiac Death (SCD)
Young athletes with undiagnosed myocarditis are at risk of sudden cardiac death due to malignant arrhythmias during intense physical activity. Screening with ECG and cardiac MRI is essential before resuming sports.
4. Chronic Myocarditis and Fibrosis
Persistent inflammation leads to myocardial scarring (fibrosis), reducing heart elasticity and function. This increases the risk of long-term heart failure.
5. Pericarditis (Inflammation of the Heart Lining)
Myocarditis can extend to the pericardium, causing pericarditis (chest pain, pericardial effusion) or even tamponade (a life-threatening fluid buildup requiring drainage).
6. Thromboembolic Complications
A weakened heart increases the risk of blood clots forming in the heart chambers, which can travel to the brain (stroke) or lungs (pulmonary embolism). Anticoagulants may be needed.
Myocarditis is a complex condition that requires prompt attention. Recognizing the symptoms, understanding the causes, and seeking early diagnosis and treatment can significantly improve outcomes. While some cases resolve with minimal intervention, others demand long-term care. By staying informed and taking preventive measures, you can protect your heart health and reduce risks.
If you or someone you know experiences unexplained chest pain, fatigue, or heart irregularities, consult a doctor immediately—early action can save lives.
The recovery time for myocarditis (inflammation of the heart muscle) varies depending on the severity and cause. Mild cases may resolve within a few weeks to months with proper rest and treatment. Severe cases, especially those leading to heart failure or chronic inflammation, may take several months or even years to recover fully. In some cases, myocarditis can cause permanent damage, requiring long-term management. Early diagnosis and treatment improve recovery chances.
Most people with mild myocarditis recover fully and have a normal life expectancy if treated properly. However, severe myocarditis (especially if it leads to heart failure or cardiomyopathy) can reduce life expectancy. Studies show that 90% of mild cases recover, while severe cases may have a 5-year survival rate of 50-70% if complications like heart failure develop. Early medical intervention is crucial for improving outcomes.
Preventing myocarditis involves reducing risk factors:
Avoid viral infections (flu, COVID-19, Coxsackievirus) through vaccination and hygiene.
Treat infections promptly to prevent heart complications.
Limit alcohol and avoid drugs (like cocaine) that can damage the heart.
Manage autoimmune conditions (like lupus) with proper medical care.
Practice heart-healthy habits (exercise, balanced diet, no smoking).
There is no single "cure," but treatment focuses on:
Rest and reduced physical activity to ease heart strain.
Medications like NSAIDs (for inflammation), beta-blockers, ACE inhibitors (for heart function), or immunosuppressants (if autoimmune-related).
Severe cases may require IV medications, a ventricular assist device (VAD), or even a heart transplant.
Treating the underlying cause (e.g., antivirals for infections).
Natural ways to lower heart inflammation include:
Anti-inflammatory diet: Omega-3s (fatty fish, flaxseeds), turmeric, ginger, leafy greens.
Exercise moderately: Regular, gentle activity improves circulation.
Stress management: Yoga, meditation (chronic stress worsens inflammation).
Sleep well: 7-9 hours nightly to support healing.
Avoid processed foods and sugar, which increase inflammation.
Strengthening the heart involves:
Aerobic exercise (walking, swimming, cycling) 150 mins/week.
Strength training (2x/week) to improve circulation.
Heart-healthy diet: Fiber, lean proteins, healthy fats (avocados, nuts).
Quit smoking and limit alcohol.
Control blood pressure and cholesterol to reduce strain.
Low-to-moderate intensity exercises are best:
Walking (30 mins/day) lowers inflammatory markers.
Swimming (gentle on joints, improves circulation).
Yoga and Tai Chi (reduce stress-related inflammation).
Cycling (boosts heart health without overexertion).
Avoid excessive high-intensity workouts, which may worsen inflammation.
While major changes take longer, you can lower cholesterol slightly in a week by:
Eating soluble fiber (oats, beans, apples) to bind cholesterol.
Cutting trans fats & saturated fats (fried foods, red meat).
Adding healthy fats (avocados, olive oil, nuts).
Exercising daily (even brisk walking helps).
Drinking green tea (contains antioxidants that help).
Yes! Bananas contain soluble fiber (pectin), which helps remove cholesterol from the body. They also provide potassium, which supports heart health by regulating blood pressure. However, they should be part of a balanced diet with other fiber-rich foods.
The fastest ways to lower cholesterol include:
Prescription statins (for rapid reduction under doctor’s guidance).
Niacin (Vitamin B3) – can lower LDL but consult a doctor.
Soluble fiber supplements (psyllium husk).
Plant sterols/stanols (found in fortified foods).
Lifestyle changes (diet, exercise, no smoking).
Several drinks help lower cholesterol:
Green tea (rich in catechins, reduces LDL).
Oat milk or soy milk (contains beta-glucans).
Pomegranate juice (antioxidants improve artery health).
Cranberry juice (boosts HDL, lowers LDL).
Water with lemon (helps flush toxins).