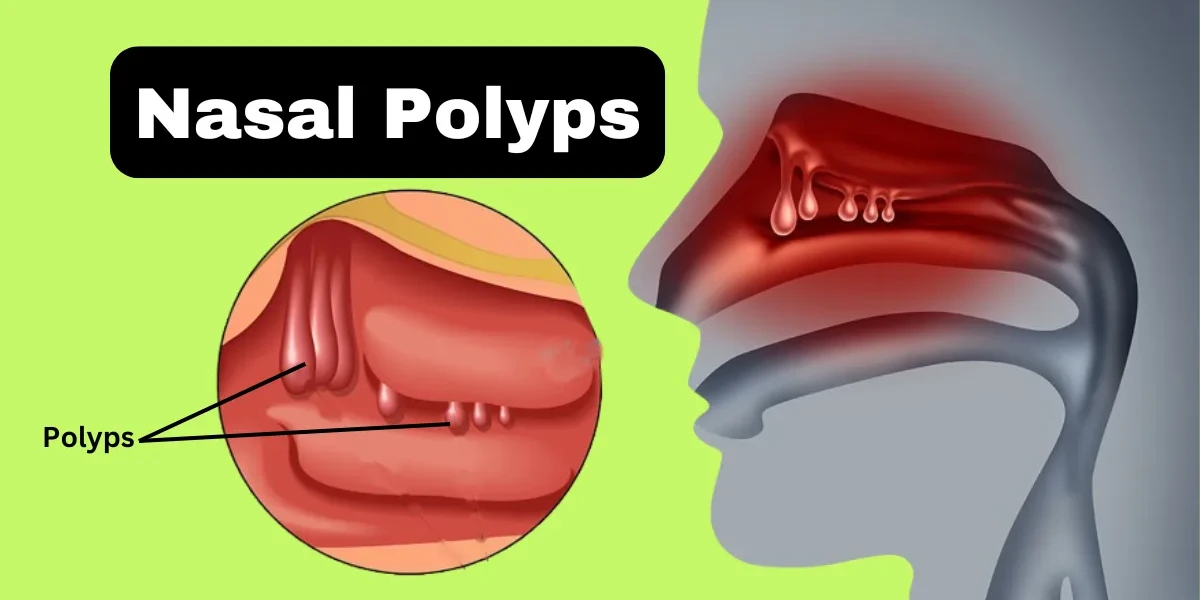
Nasal polyps are soft, painless, noncancerous growths that develop in the lining of the nasal passages or sinuses. These teardrop-shaped swellings result from chronic inflammation and can vary in size. While small polyps may go unnoticed, larger ones can block nasal passages, leading to breathing difficulties, frequent infections, and a reduced sense of smell.
Nasal polyps are soft, painless, noncancerous growths that develop on the lining of the nasal passages or sinuses. These teardrop-shaped swellings result from chronic inflammation, often due to conditions like asthma, allergies, recurring infections, or immune disorders. While small polyps may not cause noticeable symptoms, larger ones can block nasal passages, leading to breathing difficulties, reduced sense of smell, frequent sinus infections, and a persistent runny nose. Nasal polyps can affect anyone but are more common in adults, particularly those with underlying respiratory conditions. Treatment options range from medications like corticosteroids to surgical removal in severe cases.
Nasal polyps are generally categorized into two main types based on their origin and characteristics: antrochoanal polyps and ethmoidal polyps.
Antrochoanal Polyps – These polyps typically originate in the maxillary sinus (one of the cheek sinuses) and extend into the nasal cavity and nasopharynx. They are less common than ethmoidal polyps and usually occur on one side of the nose. Antrochoanal polyps are more frequently found in younger individuals and are often associated with sinus infections. Due to their location, they can cause nasal obstruction, postnasal drip, and sometimes snoring or sleep disturbances.
Ethmoidal Polyps – These polyps develop from the ethmoid sinuses, located between the eyes and nose, and tend to grow in clusters. Unlike antrochoanal polyps, they often affect both nostrils and are more common in adults with chronic inflammatory conditions such as asthma, allergies, or aspirin sensitivity. Ethmoidal polyps can lead to congestion, loss of smell, facial pressure, and recurrent sinus infections. Since they grow in groups, they may require long-term medical management or surgery if they become large or persistent.
Understanding the type of nasal polyp helps determine the most effective treatment approach, whether through medication, lifestyle changes, or surgical intervention.
Nasal polyps often develop gradually, and their symptoms can be mistaken for allergies or a common cold. However, unlike temporary congestion, nasal polyps cause persistent issues that worsen over time if left untreated. Below is a deeper exploration of the key symptoms and signs associated with this condition.
1. Persistent Nasal Congestion:
One of the most common signs of nasal polyps is a constant feeling of stuffiness. Unlike congestion from a cold, which improves within a week or two, nasal polyp blockage does not go away on its own. The nasal polyps create a physical blockage in the airways, hindering normal nasal breathing. Some people may find themselves relying on mouth breathing, especially at night, which can lead to dry mouth and throat irritation.
2. Runny Nose and Postnasal Drip:
Many people with nasal polyps experience a chronic runny nose, often with clear or slightly colored mucus. This happens because the polyps irritate the nasal lining, causing excess mucus production. Additionally, postnasal drip—where mucus drains down the throat—can lead to a persistent cough, throat clearing, or even a sore throat. In some cases, this can contribute to bad breath (halitosis) due to bacteria buildup.
3. Loss or Reduction in Sense of Smell (Anosmia/Hyposmia):
Since nasal polyps block the upper nasal cavity—where smell receptors are located—many sufferers notice a diminished or completely lost sense of smell (anosmia). This can also affect taste, as smell plays a crucial role in flavor perception. Some people only realize they have polyps when they suddenly can’t smell their food or favorite scents anymore. In rare cases, this loss can become permanent if the polyps cause long-term damage to olfactory nerves.
4. Facial Pressure and Sinus Pain:
When polyps grow large enough, they can trap mucus in the sinuses, leading to increased pressure and discomfort. This often feels like a dull ache in the forehead, cheeks, or between the eyes—similar to a sinus infection. Some people also experience headaches, particularly around the sinuses or at the base of the skull. Unlike migraines, this pain usually worsens when bending forward or lying down.
5. Snoring and Sleep Disturbances:
Obstructed nasal passages force people to breathe through their mouths while sleeping, which can lead to loud snoring. In more severe cases, nasal polyps contribute to sleep apnea, a condition where breathing repeatedly stops and starts during sleep. Poor sleep quality due to these disruptions can result in daytime fatigue, difficulty concentrating, and even mood changes.
6. Frequent Sinus Infections (Chronic Sinusitis)
Because polyps block proper sinus drainage, mucus builds up, creating an ideal environment for bacterial growth. This leads to recurrent sinus infections, characterized by thick yellow or green mucus, fever, and worsening facial pain. Unlike acute sinusitis (which lasts a few weeks), chronic sinusitis caused by polyps persists for 12 weeks or longer, despite treatment.
7. Voice Changes (Nasal Speech):
Some individuals with large nasal polyps develop a "nasal" voice, where they sound congested even when they don’t have a cold. This happens because airflow through the nose is restricted, altering vocal resonance.
If you experience prolonged nasal congestion, loss of smell, recurring sinus infections, or sleep disturbances, it’s important to consult an ENT specialist. Early diagnosis and treatment can prevent complications like chronic sinusitis, asthma flare-ups, or structural changes in the nasal passages.
asal polyps develop due to long-term inflammation in the nasal passages and sinuses, but the exact reason why some people develop them while others don’t remains unclear. Researchers believe that a combination of genetic, immune, and environmental factors plays a role. Below, we explore the key causes and risk factors in detail.
Chronic Inflammation and Immune Response: The primary underlying cause of nasal polyps is chronic inflammation of the nasal and sinus lining. When the mucous membranes are repeatedly irritated, they swell and may eventually form polyps. This inflammation can be triggered by:
Recurrent sinus infections – Frequent bacterial or viral sinusitis keeps the nasal tissues inflamed.
Allergic reactions – Allergens like pollen, dust mites, or pet dander can cause persistent swelling.
Fungal sinus infections – Some studies suggest that an abnormal immune response to fungi in the sinuses may contribute.
Asthma and Aspirin Sensitivity: People with asthma are at a higher risk of developing nasal polyps because both conditions involve chronic inflammation of the airways. A specific subset of patients has aspirin-exacerbated respiratory disease (AERD), also known as Samter’s triad, which includes:
Asthma
Nasal polyps
Severe reaction to aspirin or NSAIDs (leading to sudden asthma attacks or polyp growth)
In these cases, avoiding aspirin and related drugs is crucial to preventing polyp recurrence.
Allergic Rhinitis (Hay Fever) – Allergies to pollen, dust mites, or pet dander can cause prolonged nasal inflammation, increasing the risk of polyps. The immune system’s response to allergens leads to swelling and polyp formation in some individuals.
Aspirin Sensitivity (AERD – Aspirin-Exacerbated Respiratory Disease) – Also known as Samter’s triad, this condition involves asthma, nasal polyps, and an adverse reaction to aspirin or NSAIDs (nonsteroidal anti-inflammatory drugs). Patients with AERD often experience severe nasal polyp recurrence and require specialized treatment.
Cystic Fibrosis – This genetic disorder leads to the production of thick, sticky mucus, which can block sinus passages and cause chronic infections. Nasal polyps are common in cystic fibrosis patients due to persistent inflammation and mucus buildup.
Churg-Strauss Syndrome (Eosinophilic Granulomatosis with Polyangiitis, EGPA) – A rare autoimmune disorder that causes blood vessel inflammation, leading to asthma, sinusitis, and nasal polyps. Elevated eosinophil levels (a type of white blood cell) contribute to polyp formation in these patients.
Fungal Sinusitis – Some cases of chronic sinusitis are triggered by an immune response to fungal elements in the sinuses, leading to inflammation and polyp growth.
Genetic Predisposition – Family history plays a role, as some individuals may inherit a tendency toward chronic inflammation or abnormal immune responses that promote polyp formation.
While the causes focus on the biological mechanisms behind polyp formation, risk factors are conditions or behaviors that increase the likelihood of developing nasal polyps:
Age – Nasal polyps are more common in young and middle-aged adults, though they can occur at any age.
Sex – Men are more likely to develop nasal polyps than women.
Pre-existing Respiratory Conditions – Asthma, chronic sinusitis, and allergic rhinitis significantly increase the risk.
Vitamin D Deficiency – Some studies suggest that low vitamin D levels may contribute to chronic inflammation and polyp formation.
Smoking and Air Pollution – Exposure to irritants can worsen nasal inflammation and increase the risk of polyps.
Recurrent Infections – Frequent sinus infections keep the nasal passages inflamed, promoting polyp growth.
Immune System Dysregulation – Conditions like HIV or autoimmune diseases can alter immune responses, increasing susceptibility to polyps.
Rare conditions like Churg-Strauss syndrome (a type of vasculitis) and other autoimmune disorders can cause abnormal inflammation in blood vessels, including those in the nose, leading to polyp formation.
Nasal polyps are non-cancerous growths that develop in the lining of the nasal passages or sinuses. They are often associated with chronic inflammation due to conditions like asthma, allergies, or chronic sinusitis. The progression of nasal polyps is typically categorized into different stages based on their size, symptoms, and impact on nasal function. Understanding these stages helps in determining the appropriate treatment approach.
In the early stage, nasal polyps are small and may not cause noticeable symptoms. Patients might experience mild nasal congestion, occasional runny nose, or a slight reduction in the sense of smell. At this stage, polyps are often detected incidentally during a routine nasal examination or imaging for other conditions. Treatment usually involves nasal corticosteroids or antihistamines to reduce inflammation and prevent further growth. Lifestyle modifications, such as avoiding allergens and irritants, can also help manage symptoms.
As polyps grow larger, they begin to obstruct nasal passages more significantly. Symptoms become more pronounced, including persistent nasal congestion, postnasal drip, facial pressure, and a diminished sense of taste and smell. Some patients may develop recurrent sinus infections due to blocked sinus drainage. At this stage, doctors may recommend stronger corticosteroid sprays, oral steroids, or saline irrigations to shrink the polyps. If medical therapy fails, minimally invasive procedures like polypectomy (removal of polyps) may be considered.
In advanced cases, nasal polyps become large enough to cause severe blockage, leading to chronic sinusitis, breathing difficulties, and frequent infections. Patients may experience sleep disturbances, snoring, and even obstructive sleep apnea. The loss of smell (anosmia) can become permanent if left untreated. Treatment options at this stage often include a combination of oral steroids, biologic medications (such as dupilumab), and surgical intervention. Functional endoscopic sinus surgery (FESS) is commonly performed to remove polyps and restore normal sinus drainage.
Some patients experience recurrent nasal polyps even after treatment, requiring long-term management. This stage is common in individuals with underlying conditions like aspirin-exacerbated respiratory disease (AERD) or severe asthma. Continuous medical therapy, regular follow-ups with an ENT specialist, and sometimes repeat surgeries may be necessary. Biologic therapies targeting specific inflammatory pathways (e.g., IL-4, IL-13 inhibitors) have shown promise in reducing recurrence rates in refractory cases.
If you’ve been experiencing chronic nasal congestion, a reduced sense of smell, or recurring sinus infections, your doctor may suspect nasal polyps. However, since these symptoms can overlap with other conditions (like allergies or a deviated septum), a proper nasal polyps diagnosis requires a thorough evaluation. Here’s how doctors confirm the presence of polyps and determine their severity.
The first step in diagnosing nasal polyps is a detailed discussion about your symptoms and medical history. Your doctor will ask:
How long you’ve had nasal congestion or breathing difficulties
Whether you’ve noticed a loss of smell or taste
If you have a history of asthma, allergies, or frequent sinus infections
Whether you’ve taken any medications (like aspirin) that could trigger inflammation
If you’ve had previous sinus surgeries or treatments
This helps rule out other possible causes, such as viral infections or structural abnormalities.
Using a small handheld instrument called a nasal speculum, the doctor will gently widen your nostrils to check for visible polyps. While small polyps may not be seen this way, larger ones near the front of the nose can sometimes be spotted during this basic exam.
If polyps are suspected but not clearly visible, an ENT specialist (otolaryngologist) will perform a nasal endoscopy. This involves inserting a thin, flexible tube with a light and camera (endoscope) into the nasal passages. The procedure is usually done in the clinic and may involve a local anesthetic spray to minimize discomfort.
What the endoscopy reveals:
The exact size, location, and number of polyps
Whether they are blocking the sinuses or nasal passages
Signs of infection, pus, or mucus buildup
Any structural issues (like a deviated septum) contributing to the problem
This is the most accurate way to confirm nasal polyps without imaging.
If the polyps are deep inside the sinuses or if surgery is being considered, the doctor may order:
CT Scan (Computed Tomography) – Provides detailed 3D images of the sinuses, showing polyp size, spread, and any bone changes. It also helps plan surgical removal if needed.
MRI (Magnetic Resonance Imaging) – Less common but used if there’s concern about a tumor or fungal infection mimicking polyps.
These scans help determine the stage of nasal polyps (mild, moderate, or severe) and whether they’ve caused complications like sinus infections or structural changes.
Since allergies and immune disorders (like asthma or aspirin sensitivity) are linked to nasal polyps, your doctor may recommend:
Skin prick tests or blood tests to check for allergies
Blood tests for conditions like cystic fibrosis (in children) or autoimmune diseases (e.g., Churg-Strauss syndrome)
Identifying underlying triggers helps tailor long-term treatment.
In most cases, nasal polyps are benign (noncancerous). However, if a growth looks unusual or is only on one side, a small tissue sample (biopsy) may be taken to rule out:
Tumors (like inverted papilloma or, very rarely, cancer)
Fungal sinusitis (which can mimic polyps)
This is not routine but may be done during an endoscopy if needed.
Misdiagnosing nasal polyps can lead to ineffective treatments. For example:
Allergy medications alone won’t shrink polyps—they need corticosteroids.
Sinus infections caused by polyps will keep recurring unless the polyps are treated.
Ignoring large polyps can lead to sleep apnea or permanent smell loss.
Once diagnosed, your doctor will discuss treatment options—usually starting with nasal corticosteroids or oral steroids for severe cases. If medications fail, surgery (FESS) may be recommended.
Treating nasal polyps typically involves a combination of medications and, in some cases, surgery. The goal is to shrink the polyps, reduce inflammation, and restore normal nasal function. The best approach depends on the size of the polyps, the severity of symptoms, and whether the condition keeps coming back.
Corticosteroid Nasal Sprays
These are usually the first line of treatment. Corticosteroid sprays, such as fluticasone (Flonase), mometasone (Nasonex), or budesonide (Rhinocort), help reduce inflammation in the nasal passages and shrink polyps over time. They are effective for mild to moderate cases and must be used consistently for weeks or months to see results. Unlike decongestant sprays, they are safe for long-term use and do not cause rebound congestion.
Oral Corticosteroids
For larger or more stubborn polyps, doctors may prescribe a short course of oral steroids like prednisone. These work faster than nasal sprays and can significantly reduce polyp size, but they are not recommended for long-term use due to potential side effects, such as weight gain, high blood pressure, and weakened bones.
Biologic Medications
In cases where nasal polyps keep returning despite treatment, newer biologic drugs like dupilumab (Dupixent) may be recommended. This injectable medication targets specific immune system proteins that contribute to chronic inflammation. It has shown promising results in reducing polyp size and improving breathing in patients with severe, recurrent nasal polyps.
Antihistamines and Allergy Medications
If allergies are contributing to nasal inflammation, antihistamines (like cetirizine or loratadine) or leukotriene modifiers (such as montelukast) may help control symptoms. While they don’t directly shrink polyps, they can reduce the allergic reactions that worsen polyp growth.
Antibiotics
If a bacterial sinus infection develops due to blocked nasal passages, antibiotics may be prescribed to clear the infection. However, they do not treat the polyps themselves.
When medications fail to provide relief, surgery may be necessary. The two most common procedures are:
Polypectomy
This is a minimally invasive procedure where a surgeon removes polyps using a small suction device or microdebrider. It’s often done under local or general anesthesia and provides immediate relief from obstruction. However, polyps can grow back if the underlying inflammation isn’t controlled.
Functional Endoscopic Sinus Surgery (FESS)
For recurring or extensive polyps, FESS is a more comprehensive approach. The surgeon uses an endoscope (a thin, flexible tube with a camera) to remove polyps and open blocked sinus passages. This improves drainage and reduces the chances of recurrence. Recovery takes a few weeks, and post-surgery steroid sprays are often prescribed to prevent regrowth.
After treatment, ongoing management is crucial to prevent polyps from returning. This includes:
Continued use of corticosteroid nasal sprays (even after symptoms improve)
Regular saline nasal rinses (to keep sinuses clear)
Monitoring for allergies or asthma flare-ups
Follow-up visits with an ENT specialist
While it may not always be possible to prevent nasal polyps entirely, certain strategies can significantly reduce the risk of their development or recurrence. Since nasal polyps are closely linked to chronic inflammation, managing underlying conditions is key.
1. Control Allergies and Asthma
Allergic rhinitis and asthma are major contributors to nasal polyp formation. If you suffer from these conditions, working with an allergist to identify triggers and sticking to prescribed medications (like antihistamines, nasal corticosteroids, or inhalers) can help minimize inflammation in the nasal passages. Immunotherapy (allergy shots) may also be beneficial for long-term allergy management.
2. Maintain Good Nasal Hygiene
Regular saline rinses (using a neti pot or nasal spray) help flush out irritants, allergens, and excess mucus, reducing the risk of chronic sinus inflammation. This is especially important for people prone to sinus infections.
3. Avoid Nasal Irritants
Smoke (both tobacco and environmental pollutants), strong chemical fumes, and dust can worsen nasal inflammation. If you smoke, quitting can drastically lower your risk. Wearing a mask in dusty or polluted environments may also help.
4. Stay Hydrated
Drinking plenty of water keeps mucus thin and flowing, preventing blockages that can lead to infections and polyp formation.
5. Treat Infections Promptly
Recurring sinus infections can contribute to polyp growth. If you have frequent sinusitis, consult a doctor to determine if antibiotics, antifungals, or other treatments are needed.
6. Monitor Aspirin Sensitivity
Some people develop nasal polyps after taking aspirin or NSAIDs. If you experience worsening nasal congestion after using these medications, consult your doctor for alternatives.
While these steps don’t guarantee prevention, they can lower the likelihood of polyps forming or returning after treatment.
If left untreated, nasal polyps can lead to several complications, some of which may significantly impact health and quality of life.
1. Chronic Sinus Infections (Sinusitis)
Large polyps block proper sinus drainage, trapping mucus and bacteria. This creates a breeding ground for infections, leading to persistent sinusitis with symptoms like facial pain, thick nasal discharge, and fatigue.
2. Obstructive Sleep Apnea (OSA)
When polyps obstruct nasal airflow, breathing becomes difficult, especially at night. This can lead to snoring, interrupted sleep, and even sleep apnea—a condition where breathing repeatedly stops and starts, increasing the risk of heart disease and daytime drowsiness.
3. Worsening Asthma
Since nasal polyps and asthma are often linked, uncontrolled polyps can trigger asthma flare-ups, making breathing even more difficult. Proper polyp management can help stabilize asthma symptoms.
4. Loss or Reduction of Smell (Anosmia/Hyposmia)
Prolonged nasal obstruction can damage olfactory nerves, leading to a permanent loss of smell in some cases. This not only affects taste but also safety (e.g., inability to detect smoke or spoiled food).
5. Structural Changes (Rare but Serious)
In extreme, long-term cases, large polyps can widen the nasal bridge or even alter facial bone structure due to constant pressure. This is uncommon but may require surgical correction.
6. Spread of Infection
In rare instances, untreated sinus infections caused by polyps can spread to the eyes (causing vision problems) or even the brain (leading to meningitis).
Nasal polyps, while usually benign, can significantly impact quality of life. Recognizing nasal polyps symptoms and signs early and seeking medical advice can prevent complications. With proper diagnosis, treatment, and prevention strategies, most people can manage this condition effectively.
If you experience persistent nasal congestion, loss of smell, or recurring sinus infections, consult a specialist to explore your options. Early intervention is key to breathing easier and staying healthy.
1. What is the main reason for nasal polyps?
Nasal polyps are soft, non-cancerous growths that form in the lining of your nasal passages or sinuses. The main cause of nasal polyps is chronic inflammation due to conditions like allergies, asthma, chronic sinus infections, or sensitivity to aspirin. They develop when the mucous membrane becomes inflamed and swells over time, forming small teardrop-shaped growths. People with immune disorders or frequent sinus issues are more likely to develop them.
2. How do I get rid of my nasal polyps?
Treatment for nasal polyps usually begins with medications like nasal corticosteroid sprays (e.g., fluticasone or mometasone) to reduce inflammation and shrink the polyps. In more severe cases, oral steroids or even surgery may be necessary. Functional endoscopic sinus surgery (FESS) is a common procedure to remove larger or recurring polyps. Maintaining good nasal hygiene and managing allergies can help prevent them from coming back.
3. Can nasal polyps be serious?
While nasal polyps are not cancerous and are generally not life-threatening, they can become serious if they cause persistent sinus infections, breathing difficulties, or obstructive sleep apnea. If left untreated, they can grow large enough to block your nasal passages completely, leading to chronic discomfort, poor sleep, and reduced sense of smell or taste.
4. Can you feel nasal polyps with your finger?
In most cases, nasal polyps cannot be felt with a finger, especially if they are located deep inside the nasal passages or sinuses. They are soft and painless, so unless a polyp is large and near the nostril opening, you likely won’t notice it by touch. Diagnosing them typically requires a nasal endoscopy performed by an ENT specialist.
5. How to check for nasal polyps at home?
At home, it’s difficult to definitively diagnose nasal polyps. However, symptoms like chronic nasal congestion, reduced sense of smell, postnasal drip, and a feeling of pressure around the forehead or cheeks could be clues. If these symptoms persist despite using over-the-counter treatments, it’s important to consult a doctor who can confirm the presence of polyps using imaging tests or a scope.
6. Why is one nostril always blocked?
It’s normal for nostrils to alternate airflow due to something called the “nasal cycle.” However, if one nostril is constantly blocked, it might be due to a deviated septum, enlarged turbinates, allergies, or nasal polyps. A deviated septum — where the cartilage dividing your nostrils is off-center — is a common cause of chronic one-sided congestion.
7. How to unblock nose at night?
To unblock your nose at night, try using a humidifier, saline nasal sprays, or a warm compress over your sinuses. Elevating your head while sleeping and using nasal strips can also help improve airflow. If allergies are a cause, antihistamines or decongestants may offer relief. Avoiding allergens like dust mites and keeping your bedroom air clean can also be effective.
8. What do nasal polyps look like?
Nasal polyps appear as pale, grayish, or pinkish grape-like swellings inside the nasal passages. They are usually soft and non-tender. On medical examination, they may be seen hanging or clustered in the nasal cavity. If they’re visible near the nostrils, they may look like small, smooth bumps, but they’re often deeper in the sinuses.
9. How to fix uneven nostrils naturally?
Uneven nostrils are often due to asymmetrical cartilage or a deviated septum. While there are no guaranteed natural methods to change nostril shape, certain facial exercises and breathing techniques may slightly tone the surrounding muscles. However, significant asymmetry typically requires medical intervention such as septoplasty or rhinoplasty to correct.
10. Which nose shape is most attractive?
Attractiveness is subjective and varies across cultures, but studies suggest that symmetrical noses with soft contours and a well-balanced nasal tip are generally seen as more aesthetically pleasing. The “Greek nose” — straight with no bumps — and the “button nose” — small with a slight upturn — are often considered attractive. However, beauty standards vary, and confidence plays a big role.
11. How do you self-test for a deviated septum?
You can try a simple self-check by closing one nostril and breathing through the other. Then repeat on the opposite side. If one side feels significantly more blocked, and this remains constant, it may indicate a deviated septum. Other signs include chronic nasal congestion, frequent sinus infections, or noisy breathing during sleep. A proper diagnosis requires a physical exam by a doctor.
12. How much does septoplasty cost?
The cost of septoplasty varies depending on your location, insurance, and the complexity of the surgery. In the U.S., the out-of-pocket cost can range from $3,000 to $10,000 without insurance. If it’s deemed medically necessary (for example, to improve breathing), insurance may cover part or all of the procedure. Always consult your provider for a detailed quote and pre-authorization.